Esophagostomy Tube
Esophagostomy tubes (E-tubes) are used in hyporexic and anorexic patients to provide enteral nutrition.
Summary of the Procedure:
| Indications | Nutritional and/or fluid support; can also be used to aid in medication delivery. |
| Limitations | Smaller lumen compared to gastric feeding tubes, therefore a watery consistency of food is needed (E.g., Hill’s a/d or Medi-cal Recovery Formula blended with water; Boost or Emeraid liquid). Patients with vomiting can displace the tube. |
| Complications | Most commonly infection around stoma,
Less common: Esophageal/gastric irritation, vomiting if tube is extended through the lower esophageal sphincter. |
| Contraindications | Refractory vomiting, regurgitation, megaesophagus, patients with decreased conscious protection of the airway. |
| Supplies/instruments | Surgical prep/scrub, sterile gloves
Red rubber catheters or similar tubes (usually 10-20 French diameter; 14-16 French tubes are suitable for most cats) Scalpel blade Carmalt forceps Sterile lubricant Needle holders, non-absorbable suture Bandage material (gauze squares & cling, cotton roll, Vetrap or similar elastic outer wrap |
| Position | Most commonly right lateral recumbency. |
| Restraint | General anesthesia |
Landmarks:
- The esophagus courses slightly left and dorsal to the trachea. For this reason, the tube is often placed on the left side. However, it is possible (and not difficult) to place the tube on the right side of the neck if you have reasons to do so (e.g., wound or other abnormality on the left side)
- Measure the distance from the approximate entry site in the mid-cervical region to the level of the 7th intercostal space.
- Identify the position of the jugular vein by holding the vein off at the level of the thoracic inlet; avoid this area when planning the tube insertion site (site is usually dorsal to jugular vein).
When do you place an esophagostomy (E) tube versus a nasoesophageal (NE) or nasogastric (NG) tube?
- E-tubes are more securely placed than NE/NG tubes – E tubes can be used by pet owners at home, versus NG and NE tubes which are generally used only in hospital environments and can be removed by the patient fairly easily.
- E-tubes are larger in diameter than NE or NG tubes, allowing a blended slurry of canned food & water to be used rather than special liquid diets that are needed for the smaller diameter NE and NG tubes.
- You might have a patient start with an NE/NG tube in hospital for a few days, become more stable for anesthesia, then place an E tube (removing the NE/NG tube) so that you can send the patient home if at-home care is feasible for continued recovery.
Details of the Procedure:
- Anaesthetize the patient and place the patient in right lateral recumbency. Intubation is recommended even if injectable anesthetic agents are administered, to reduce risk of placing forceps in trachea. Clip & surgically prepare an area from the caudal ramus of the mandible caudally to the thoracic inlet, dorsally and ventrally to midline.
- Pre-measure the feeding tube from level of the 7th intercostal space to the approximate point of insertion, and mark the tube. Some clinicians prefer to cut the distal end of the tube to increase its diameter.
- Place a sterile drape over the cervical region, with the surgically prepared area exposed.
- Gently pull the tongue rostrally, and have an assistant insert the Carmalt forceps (with closed tips) into the mouth and down the esophagus.
- Palpate the tips of the Carmalt forceps through the skin in the mid-cervical region. Gently incise the skin and fascia overlying the forceps. The incision should be small (0.5 cm) and parallel to the esophagus.
- The esophagus should be visible through this incision as a thin tissue (often will appear clear or transparent) overlying the forceps. Make a tiny incision in the esophageal wall over the forceps while the assistant places gentle pressure on the forceps to “pop” the tips through this incision.
- Place sterile lubricant on the distal end of the feeding tube, then insert the tip of the tube into the open Carmalt forceps (tip of tube flush with the ends of the forceps to facilitate passage).
- Pull the forceps with the tube rostrally out the mouth. Ensure that oral or esophageal tissues are not entrapped in the forceps, which will prevent you from easily pulling the tube rostrally. As the distal tip of the tube is pulled out of the mouth, note that the proximal end of the tube is oriented caudally. Do not pull the tube completely through the incision in the mid-cervical area. Small forceps can be used to clamp off the proximal end of the tube.
- Unclamp the distal end of the tube from the forceps. Bend the distal end of the tube over on itself to create a “U-turn.” Use your fingers or the forceps to push the distal end of the tube down the esophagus. The proximal end of the tube will “flip” itself rostrally when the distal end of the tube has been placed in the esophagus appropriately.
- Manipulate the tube gently so that the placement marker is at the point of insertion. This will allow the tube to be at approximately the appropriate level.
- Place a purse-string suture around the entry site of the tube, leaving the ends long to allow for a finger-trap suture to be performed. An anchor suture that incorporates the periosteum of the atlas is also performed by some clinicians to secure the tube in place. This may be useful in larger patients.
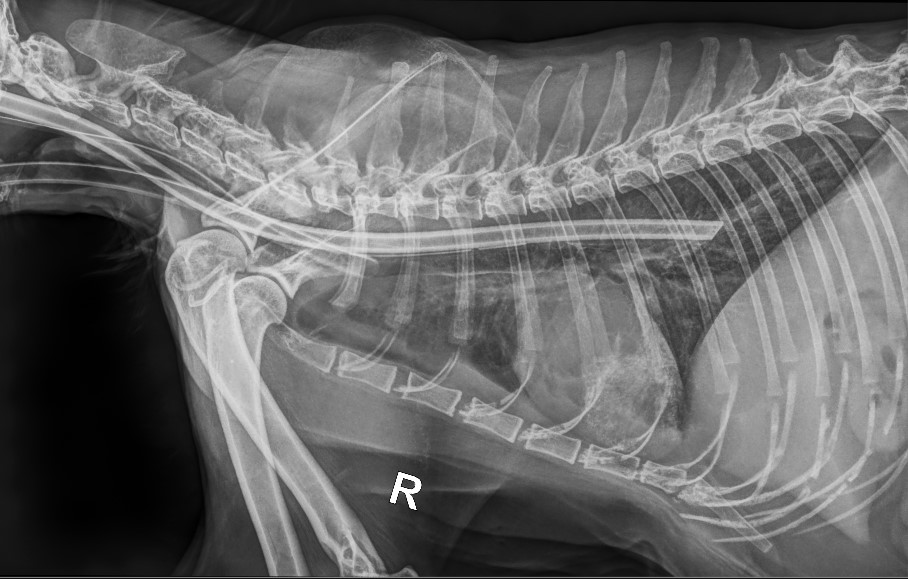
- Take a radiograph to ensure correct placement of the tube in the esophagus. Adjust the length of the tube if necessary.
- Place a neck wrap (4×4 gauze square with an incision in it to place around the tube, followed by soft cotton roll, then gauze cling, and finally Vetrap or another elastic outer bandage).
Alternative Technique:
This technique requires a trocar device produced by Mila International. It allows the clinician to place the tube directly down the esophagus after making the incision, rather than going through the steps of bringing the E-tube out of the mouth and flipping it back down the esophagus: