Cardiac Regulation
Cardiac regulation is constantly working to ensure sufficient blood flow supply is sent around the body. When we exercise, we increase cardiac output so our muscles can get the oxygen they need. When we sleep, cardiac output is decreased as our body is resting. This section will explore the various regulated variables that influence cardiac output and how they can be manipulated. We will discuss how both intrinsic and extrinsic controls affect cardiac output, and ultimately, blood pressure. But before we get into that, let’s review the cardiac cycle.
Learning Outcomes
In this section you will learn…
- How end diastolic volume is regulated by preload.
- The many methods of regulation for end systolic volume and heart rate.
- To apply the cardiac output formula and how each variable can be manipulated to affect cardiac output.
Overview
The Cardiac Cycle
To begin this section, let’s review the following diagram as it visually depicts the stages of the cardiac cycle. This figure provides a strong review of several previous sections to refresh your knowledge before introducing new concepts. Review the phases of the cycle, the anatomical structures found within the heart, and the pathway of blood flow into, within, and out of the heart’s chambers.
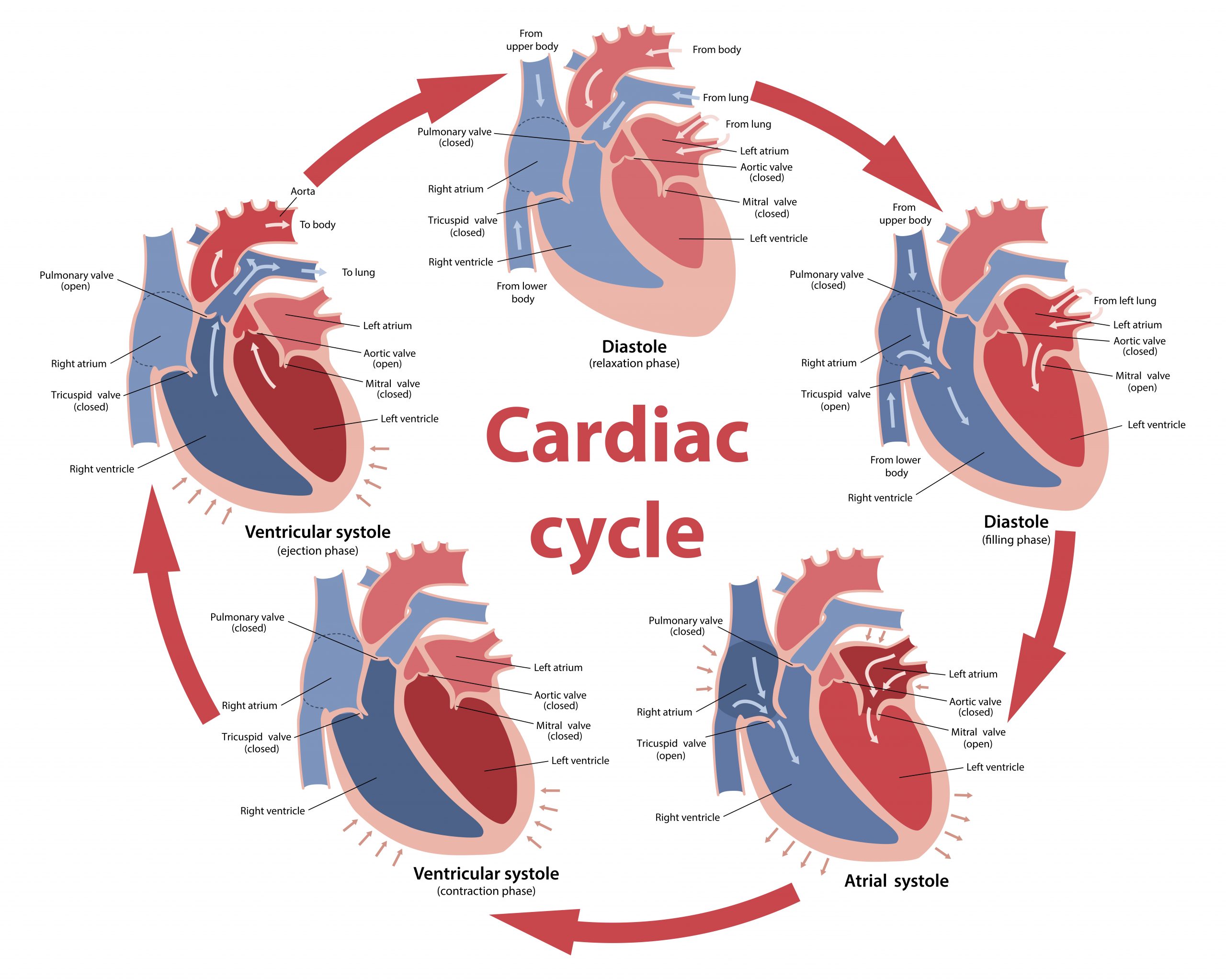
To summarize the figure the heart pumps at a relatively stable rate of cardiac cycles, denoted as HR (heart rate). An individual cardiac cycle begins following contraction, causing blood to be ejected from the left ventricle, otherwise known as the phase of systole. The volume remaining in the ventricle after systole is the end-systolic volume (ESV). The ventricles relax, and the atria contracts causing the atrioventricular valves to open as the atria pressure exceeds the pressure in the ventricles. Once the ventricles have been sufficiently filled, the pressure in the ventricles will be greater than the pressure in the atria, and the atrioventricular valves will shut to prevent back-flow. The amount of blood present within the left ventricle after filling represents the end-diastolic volume (EDV). The ventricles undergo iso-volumetric contraction, which causes pressure within the ventricle to rise until it exceeds the pressure in the aorta. At this point, the left ventricular pressure has exceeded the afterload, and the aortic valve will open, allowing blood to be ejected into circulation. This concludes one complete cardiac cycle.
The difference between EDV and ESV is the total volume of blood pumped, which represents SV (stroke volume). CO (cardiac output) is the combination of the total amount of blood pumped each cardiac cycle (SV) and the number of cycles per unit time (HR). Therefore CO is the product of SV and HR, and it is recorded in litres per minute (L/min).
[latex]CO= SV*HR[/latex]
Summary of Factors Affecting Cardiac Output
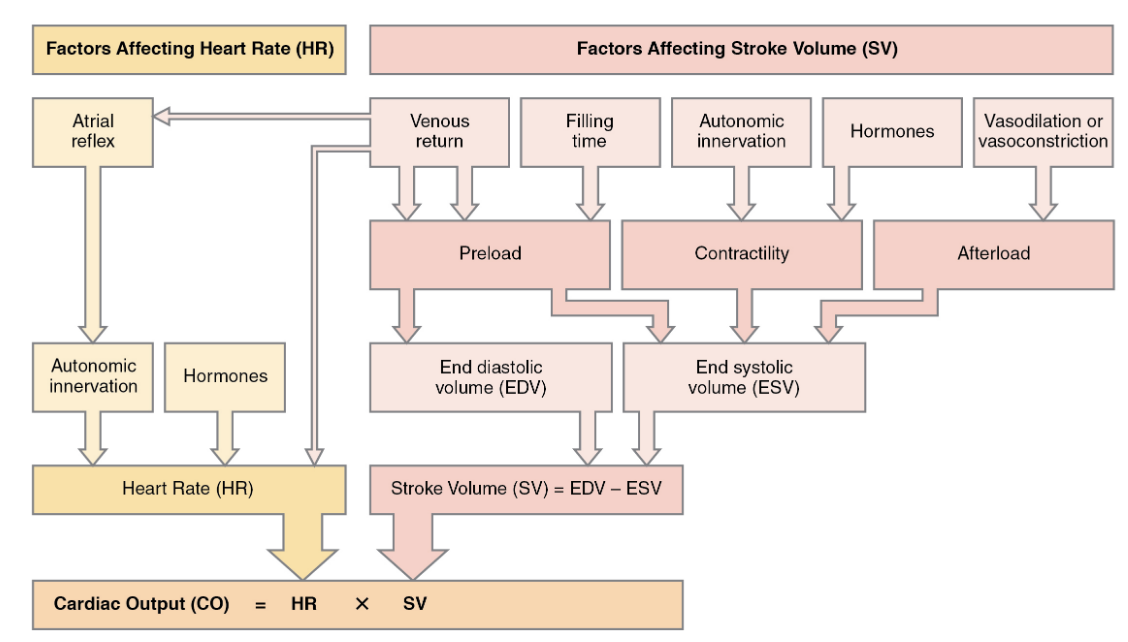
Due to the relationship discussed above, we can appreciate that any factors that affect HR and SV will affect CO. The flow chart below provides an in-depth description of several factors that influence HR and SV and how this will alter the CO of the heart. We can also see the regulators of ESV and HR that will be discussed in further detail later in this section. Additionally, use this diagram to understand how preload affects EDV as it will not be discussed in further detail.
Summary of Factors Affecting Stroke Volume
The table below highlights how preload, contractility, and afterload can influence EDV and ESV, and therefore, CO. It will help you understand what can raise or lower these factors, so make sure you understand the material presented below.
| Factors Affecting Stroke Volume | Preload | Contractility | Afterload |
|---|---|---|---|
| Increased Stroke Volume due to: |
|
|
|
| Results in: | Increased EDV and SV. | Decreased ESV and increased SV. | Increased ESV and decreased SV. |
| Decreased Stroke Volume due to: |
|
|
|
| Results in: | Decreased EDV and SV. | Increased ESV and decreased SV. | Decreased ESV and increased SV. |
Make sure you understand the definitions of each of the variables included in the previous diagram instead of just memorizing them.
Test Your Knowledge
Clinical Application:
Atrial fibrillation is an irregular heartbeat caused by an electrical disturbance in the heart. This electrical disturbance causes the ventricles to contract faster than usual. What would happen to preload as a result of atrial fibrillation? How would this change in preload affect EDV and CO? [2] Hint: Recall how increasing HR influences the proper filling of the ventricles in diastole.
To learn more about the affects of the heart, read atrial fibrillation.
Intrinsic Control of ESV
Frank-Starling Law of the Heart
The Frank-Starling law of the heart describes the relationship between ventricle stretch and contraction strength. The law suggests that as we increase the left ventricle’s filling before contraction, otherwise known as EDV or preload, the cardiac myocytes will lengthen their sarcomeres, and a more powerful contraction will occur. The concept of lengthening the sarcomeres due to tension was also seen in the skeletal muscle fibers. However, the skeletal muscle cells yield a specific sarcomere length in which optimal contraction will occur. Any increases or decreases beyond this optimal point will decrease the force of contraction. Cardiac myocytes do not share this characteristic as they are not structurally set to have an optimal contraction. It is only if the sarcomeres experience extreme lengthening that adverse impacts will occur, causing contraction to decrease.
This video was explains the mechanism of contraction of sarcomeres in the heart. Additionally, this video provides background information on the graph done in class comparing force (SV) and stretch (EDV) to explain the intrinsic control of ESV. If you are struggling with the concept of why force is low when stretch is too low (myosin is too close to Z-disk) and when stretch is too high (myosin is too far from Z-disk), this video will provide some insight. Please note that this learning object is above material for HK*3810 due to the great detail in explaining the actions of actin and myosin in cardiac myocyte sarcomeres.
Staircase Phenomenon / Treppe Phenomenon -Frequency-dependent Activation
The Staircase or Treppe Phenomenon is a relatively complicated concept that is still under extensive scientific research. The phenomenon suggests that if cardiac myocytes are repetitively stimulated, it will cause a series of contractions that will increase in force until a maximal level is achieved. Essentially, increases in HR will cause increases in the strength of heart contractions. If contractions become more forceful, it is inferred that ESV will decrease, and more blood is being ejected from the heart during systole. This video explains the phenomenon and why an increase in the frequency of stimulation (heart rate) reflects an increase in force (contraction) using electric shock as an example.
The staircase phenomenon is a tricky concept for which there is no mechanism. What is important for this course is understanding how it influences ESV. Using the diagram drawn in class (force vs. time), try to remember that an increase in HR can cause an increase in the force of contraction, resulting in a decrease in ESV. This is because more force causes more blood to be pumped and thus less volume staying in the ventricle. This results in a reduced ESV and increased CO. The video below explores this phenomenon but is only relevant until the 1:52 minute mark.
Test Your Knowledge
Thinking Beyond:
The pericardium is a sac made up of membrane and connective tissue that surrounds the heart. It has many jobs but mainly acts as protection for the heart and reduces friction with surrounding structures. Knowing this, how does the pericardium influence the intrinsic relationship between SV and EDV? What would happen if the pericardium was removed? Hint: Think about the Frank-Starling Law of the heart.
Extrinsic: Neural Control of ESV and HR
Autonomic Nervous System Effects on the Heart
This video was included because it introduces HR and SV and how they are affected by Sympathetic Nervous System (SNS) input and Parasympathetic Nervous System (PNS) input. The video explains how conduction velocity and relaxation rate are also influenced by SNS and PNS, which can help explain how ESV is influenced as well. Finally, the video describes where in the heart extrinsic control acts. This video is above material for HK*3810 due to the use of vocabulary.
Sympathetic and Parasympathetic Nervous Systems Effect on Cardiac Output and Blood Pressure
This video will explain how the SNS and PNS cause opposite effects on HR and SV. Due to the mathematical relationships of these variables, the systems will therefore cause opposite effects on CO and MAP (mean arterial pressure). The video provides a clear visual of the cascades for both nervous system innervations to the heart and includes an analogy about the SNS input acting as a gas pedal and the PNS input acting like the brakes of a car. This analogy provides a simplified and memorable description that may help interpret their opposing effects on the heart. Past the 5:30 mark, this video is no longer applicable to this section as it starts talking about vasculature which is addressed in the next section of this chapter.
There are many neural pathways/cascades that you are responsible for understanding in this section. It is essential to have a solid understanding of them. Try writing each step down on different scraps of paper. Mix them all up and try to reassemble the correct order without looking at your notes. Compare your work to your notes; the areas where you went wrong are the blind spots in your memory and, thus, the parts you need to understand more. If you don’t have any paper with you, try the following interactive fill-in-the-blanks!
Neural Control of ESV
Neural Control of HR
Tips From Past Students
Don’t just try to memorize the pathways of SNS and PNS regulation. Actually, go through each step, making sure you understand why that was the logical next step. For example, increasing activity of the Ca2+ (calcium) pumps on the sarcoplasmic reticulum (SR) leads to a decrease in relaxation time and an increase in the speed of contraction because those Ca2+ pumps are how we get Ca2+ back into the cytoplasm. More Ca2+ in the cytoplasm means more Ca2+ can re-enter the muscle cell and cause a contraction therefore, more contractions can occur faster (less time between contractions = increase speed of contractions).
Extrinsic: Hormonal Control of End Systolic Volume and Heart Rate
Hormonal Control of End Systolic Volume
The hormonal control of ESV produces the same result as the neural SNS stimulation. The difference between the neural SNS and hormonal control lies in the time frames of the mechanisms. The SNS mechanism functions very rapidly as there is direct neural innervation to the cardiac myocytes. The hormonal impact takes a bit longer to achieve this as the adrenal glands release the catecholamines epinephrine and norepinephrine into the bloodstream. These neurotransmitters then travel through the blood to reach the cardiac myocytes. Despite this time frame distinction, the two systems cause nearly identical cascades, and in fact, the hormonal response is initiated as a result of SNS stimulation. Consider the following cascades;
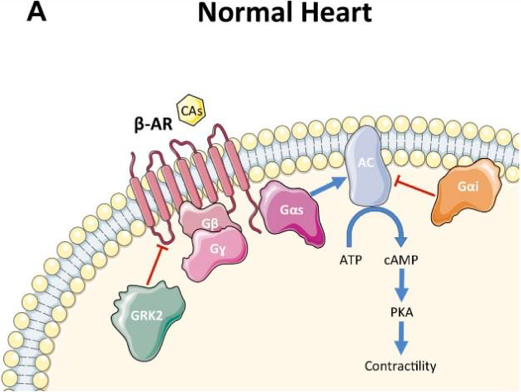
Stimulation of the SNS causes the release of norepinephrine on the cardiac myocytes where they locate the beta-adrenergic membrane receptors. Stimulation of these membrane receptors activate a stimulatory G-protien which increases acetylcholine, cyclic AMP (cAMP), and protein kinase. This cascade increases the phosphorylation of voltage-dependent calcium channels and calcium pumps on the SR. Overall, the net results of this neural cascade causes an increase in contractility due to elevated levels of trigger calcium within the cells, and an increase in calcium clearance to facilitate more contractions in a smaller amount of time.
When the SNS is stimulated, it will also cause the adrenal glands to release the catecholamine epinephrine and norepinephrine, which initiates the hormonal mechanism. The catecholamines enter the bloodstream and travel to the cardiac myocytes, where they locate the same beta-adrenergic membrane receptors. The rest of the cascade is identical to the neural mechanism. Therefore, it results in an increase in contractility through increased phosphorylation of calcium channels and activity of the calcium pumps on the sarcoplasmic reticulum.
The subsequent figure provides a visual representation of how the neural system initiates the hormonal response and the consequential cascade that occurs to increase contractility. The image demonstrates what stimulatory G-proteins and B-adrenergic membrane receptors look like at a cellular level to help understand the process. Note that you do not need to know all of the names of the stimulatory G proteins in figure 3.
The hormonal control of ESV and HR start differently than their SNS neural control counterpart, but end the same. What part of the cascade is different between the neural and the hormonal control for each variable? Check your answer in the interactive material below.
Differences Between Neural and Hormonal Control of End Systolic Volume Cascades
Differences Between Neural and Hormonal Control of Heart Rate Cascades
After doing the above exercises, you now know that there are only two small differences between neural control and hormonal control of both ESV and HR. So, then why have both methods of regulation?
Neural control is the first response (quick) to SNS stimulus, whereas hormonal control is a long and prolonged response to SNS stimulus. Together, you get a quick, initial response with neural which can back off once hormonal control kicks in for a more sustained response.
Test Your Knowledge
Real-Life Scenario:
You are strolling around the Arboretum when you realize you are going to be late for your HK*3810 lecture on the other side of campus. As you run towards the lecture hall, you experience an increase in epinephrine release. What nervous system is responsible for the release of epinephrine? What effect will the release of epinephrine have on ventricular myocyte function? Hint: Reflect back on contractility and contraction speed.
Determinants of Cardiac Output and Their Regulators
The following video offers a helpful summary of the four major determinants of CO and the factors that can alter these variables. As discussed before, variations in CO will affect MAP, which is a highly regulated variable of the body. The four CO determinants include; HR, EDV or preload, ESV, and afterload. The video goes into detail about the various factors that will impact the four variables and their resulting effect on CO. In addition to this explanation, the video discusses how the SNS and PNS input influences contractility and HR in further detail. This video is a useful review of the content covered in the section and can be used to confirm your understanding of the topics.
“Cardiovascular System Physiology – Cardiac Output (stroke volume, heart rate, preload and afterload)” by Armando Hasudungan is all rights reserved.
Tips From Past Students
To understand how ESV is regulated by afterload, you have to understand what afterload is. Afterload is defined as the load in the aorta that the ventricle has to overcome to pump blood out. Consider the scenario of a high afterload. This would mean less volume is pumped out per contraction because it needs to overcome a higher load. Since less blood is getting pumped out, more is staying in the ventricle after ejection (increased ESV). Increased ESV results in decreased SV and thus decreased CO due to the following equation:
[latex]CO = ( HR * SV)[/latex]
Regulated Variables
Regulated variables are an important and recurring concept in human physiology. In general terms, a regulated variable describes physiological conditions kept within a range to maintain homeostasis. The definition is broad because there are many types of regulated variables. The body regulates each differently; it has different mechanisms specific to physiological systems, sensors in different places, and different feedback systems that rely on hormonal, neural, or local factors.
If the concepts of sensors, effectors, regulated variables, and homeostasis are still confusing you, don’t fear. There is an amazing article that can help! The paper, A physiologist’s view of homeostasis, by Modell et al. (2015) breaks these abstract concepts into comprehensible terms and answers frequently asked questions.
Key Takeaways
Consider the following concepts to help guide your studies:
- Many factors can affect HR and SV, this will affect CO, and ultimately BP.
- Intrinsic and extrinsic control will impact the heart differently.
- SNS input acts like a gas pedal whereas PNS input acts as the brake pedal.
- Preload and EDV are considered to be the same, however, afterload and ESV are different.
- Regulated variables are a recurring concept in human physiology; the body has unique mechanisms with different sensors and feedback systems for each variable.
Subchapter Quiz
The questions below can be used to assess your knowledge within this chapter. There are five multiple-choice questions that you should attempt without referring to your notes. The questions will provide you with responses to your answers to guide your studying but should not be used as your only resource.
Media Attributions
- Cardiac Cycle © Olga Bolbot/Shutterstock.com is licensed under a CC BY (Attribution) license
- Summary of Major Factors Influencing Cardiac Output © J. Gordon Betts, Kelly A. Young, James A. Wise, Eddie Johnson, Brandon Poe, Dean H. Kruse, Oksana Korol, Jody E. Johnson, Mark Womble, Peter DeSaix is licensed under a CC BY (Attribution) license
- Beta Adrenergic Activation – Hormonal Control © Claudio De Lucio, Akito Eguchi & Walter J. Koch is licensed under a CC BY (Attribution) license
- Gordon Betts, J., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol O., Johnson, J.E., Womble, M., & DeSaix, P. (2013, April 25). 19.4 Cardiac Physiology. OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/19-4-cardiac-physiology ↵
- Staerk, L., Sherer, J. A., Ko, D., Benjamin, E. J., & Helm, R. H. (2017). Atrial Fibrillation: Epidemiology, Pathophysiology, and Clinical Outcomes. Circulation research, 120(9), 1501–1517. https://doi.org/10.1161/CIRCRESAHA.117.309732 ↵
How long the heart is in diastole. If the filling time is too quick there will be no blood to pump out, if it is too long blood will start to pool in the filling chamber.
Blood flow back to the heart within a cardiac cycle. If venous return does not equal CO it could be evidence of blood pooling or a blockage somewhere.
Not enough oxygen to properly function.
Dangerously high potassium levels in the body.
Regulation by a factor originating from within the tissue.
Regulation by factors originating outside the tissue.
Membrane protein required for neurotransmitter signalling by metabotropic receptors. Involved in regulation of ion channels and effector enzyme synthesis or breakdown.

