Vasculature
By now, you understand the anatomy of the heart and circulatory system, as you know that blood will flow from the heart into the systemic and pulmonary circulations. However, understanding the cardiac cycle and the path of blood flow is just the tip of the iceberg in the complexity that is our circulatory system. As blood flows throughout our bodies, it will pass through arteries, capillaries, and veins. Each of these vascular compartments yields different structural and functional characteristics that influence blood flow throughout the system. This chapter will explore the differences between these blood vessels and their relation to cardiac regulation.
Learning Outcomes
In this section you will learn…
- How blood flow vasculature operates and is influenced.
- The structural and functional differences between the vasculature that comprise the circulatory system.
- The concept of vasoconstriction vs. vasodilation.
Anatomy & Blood Flow
You have been introduced to some of the basic concepts regarding the anatomy of the heart and blood flow through the circulatory system. Before we begin a more in-depth discussion of the structural and functional differences of the vascular components, let’s review some of the key concepts from subchapter one:
- Pathway of Blood Flow: blood enters the right atrium through the Superior and Inferior Vena Cava→ passes from the right atrium to the right ventricle through the tricuspid valve→ pumped from the right ventricle to pulmonary arteries→ the blood flows across the lungs where it undergoes gas exchange in the pulmonary capillaries→ returns to the left atrium through the pulmonary veins → the mitral valve allows flow from the left atrium to left ventricle→ as the heart undergoes contraction the blood is pushed from the left ventricle to the aorta through the aortic valve→ the blood is then in the systemic circulation where it is delivered to the tissues.
- The right heart = blood flow to the pulmonary circulation, while the left heart = blood flow to the systemic circulation.
- Arteries carry blood away from the heart, veins carry blood towards the heart.
- Gas exchange occurs in the capillaries of the pulmonary and systemic circulations.
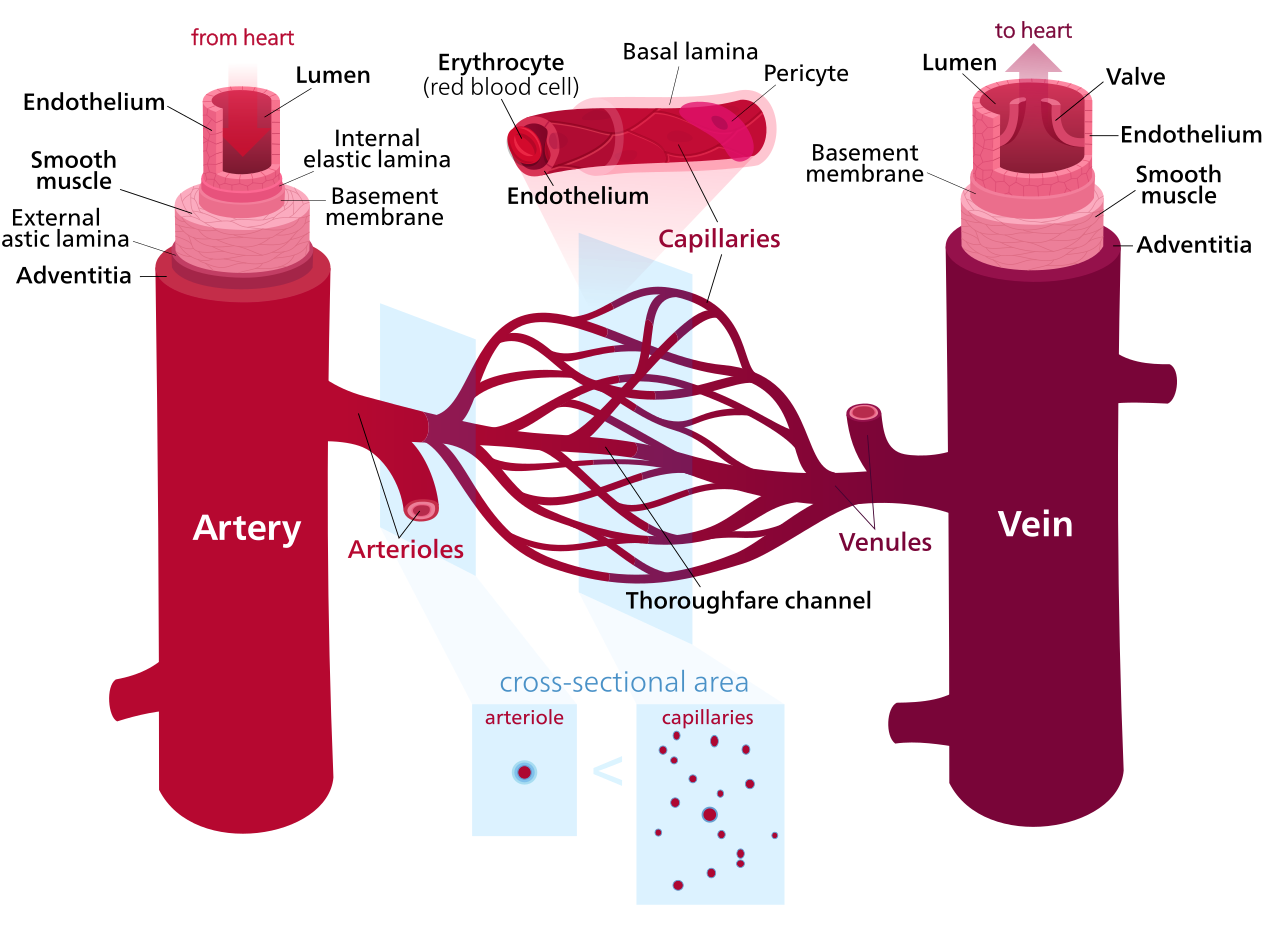
Expanding upon this knowledge, this subchapter will take a more detailed approach to discuss the structural design of the system’s vascular components. Understanding the structural differences of arteries, veins, and capillaries will help understand the vessels’ different functional roles. The diagram below depicts the structural design of an artery, a vein, and a capillary. Notice the differences between the vessels; the amount of smooth muscle integrated into the arteries, the lack of vessel layers of the capillaries, and the veins’ wider diameter.
Vasculature Diagram
The labeled diagram below offers an in-depth visual comparison between the vasculature structure of arteries, capillaries, and veins. Notice the fine detail represented in the diagram regarding the layers and cross-sectional area of the components. The two most important takeaways from this figure include the importance of the capillary cross-sectional area and the presence of smooth muscle surrounding the basement membrane in both arteries and veins.
Test Your Knowledge
Real-Life Scenario:
Create a chart to compare and contrast the differences in pressure levels and wall layers between the vascular compartments; arteries, veins, and capillaries. Consider why these differences are related to the primary functions of the compartments. Hint: Refer to figure 1 located in this sub-chapter as it provides a visual for the appearance of the three vascular components that should help you brainstorm how their structure relates to their function.
Vasculature Video
The following video is a useful source to refresh your memory on previously covered content while introducing you to new concepts regarding the characteristics of the vasculature. The first part of this video (until 4:45) will help you apply the scale of the vascular system to your understanding of the pathway of blood flow. Anything beyond 4:45 will help you understand the different properties of the various vascular components such as; arteries, arterioles, capillaries, venules, and veins. THis video is above the level of knowledge required for HK*3810.
Tips From Past Students
When learning about the different vasculature components of the circulatory system, most students will try to memorize the many different structural characteristics. Try to avoid straight memorization and instead consider a given compartment’s function and explain why the compartment’s structure supports its function. Relating the structural and functional aspects of the various types of vasculature will promote a better understanding of each compartment and the circulatory system as a whole. For example, arteries contain more elastin and collagen fibres making them MORE elastic than veins. Try and consider why this is through considering a structural-functional relationship.
Arteries and Veins
This video does a great job of relating the properties of arteries and veins discussed in the previous figure and video to their purpose within the cardiovascular system. The video’s content also relates the properties of arteries and veins to the regulation of blood pressure through nervous system innervation. To support your understanding of the nervous system influence on the regulation of blood pressure, the video offers a good explanation of vascular compliance and resistance. It is recommended to watch this video all the way through as it essentially summarizes this whole chapter and explains concepts in a different manner than you will likely learn in lecture.
Test Your Knowledge
Real-Life Scenario:
Consider the pulmonary and systemic circulations. The systemic circulation is equipped with a much more significant amount of vascular smooth muscle allowing for extreme control over resistance in the system. Why is it essential to have the systemic circulation equipped with vasculature that can be altered in resistance? Why does the pulmonary system not share these characteristics? Hint: Think about what tissues each circulation supplies.
Capillaries
The capillaries are recognized as the smallest but most abundant component of the vascular system. Within circulation, the capillaries form the connection between the arteries carrying blood away from the heart and the veins returning blood to the heart. The capillaries facilitate the essential function of gas exchange in both the pulmonary and systemic circulations. The pulmonary capillary beds found within the lungs exchange the CO2 (carbon dioxide) within the blood for the newly inhaled O2 (oxygen). The systemic capillary beds provide O2 to the body tissues while removing the CO2 produced by these tissues. Without the capillaries performing this necessary process, we would not release CO2 from the body or deliver the O2 we breathe into our body to the tissues.
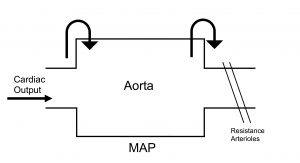
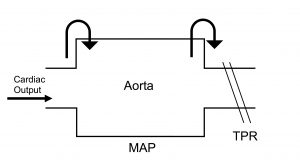
The concept of compliance and resistance can be applied to the capillaries to understand the flow into and out of the vascular compartment. Mean arterial pressure (MAP) and the resistance arterioles control the volume flowing into the capillaries, while venous pressure controls volume out of the capillaries.
Venous pressure is a concept often used synonymously with mean circulatory filling pressure (MCFP). These terms refer to the pressure within the veins and are the pressures that blood faces as it flows out of the capillaries. For a deeper understanding, read about venous pressure and venous return.
Tips From Past Students
In this unit, make sure you pay attention whenever blood pressure (BP) and cardiac output CO) are being discussed. The whole point of the heart and vasculature unit is to understand how CO is regulated to maintain blood pressure. Exam questions will ask big picture concepts, so make sure you can connect the dots.
Pressure-Volume Flow and Resistance Summary Video
This source was included because the video makes great connections between the pressure-volume relationship and vasculature. The video approaches the topic through a more mathematical and physics-based perspective that reflects how you likely learned the content in the classroom. The video also introduces the flow equation that will be the focus later in the subchapter.
Understanding the Flow Equation
The flow equation states that blood flow is dependant on the difference between pressure gradients and the resistance it will face. Through the use of this equation, we can estimate fluctuations in blood flow throughout the circulatory system. Before putting together the equation, let’s take a closer look at the variables.
Vascular resistance, denoted by R, refers to the resistance that the previous compartment must overcome to promote blood flow to the next compartment. Three mechanisms can control vascular resistance. Length and number of vessels and viscosity are two mechanisms that will not be focused on in this subchapter. Vessel radius is a very influential and rapid mechanism for altering resistance through constricting or dilating vessels and is discussed later in this subchapter.
The pressure gradient refers to the change in pressure between two compartments that blood is flowing through. As discussed in previous subchapters, the heart and circulatory systems rely on pressure gradients to promote proper directionality of blood flow. This pressure gradient is controlled by the blood flowing into the vessel and blood flowing out of the vessel. If more blood is flowing into the vessel (P1) than exiting (P2), the pressure within the vessel will increase. If more blood is leaving the vessel (P2) than entering (P1), the pressure will decrease.
[latex]Q = \frac{(P1 - P2)}{R}[/latex]
Flow Example: Arteries
In any compartment, flow through the vessel is controlled via [latex]Q = \frac{(P1 - P2)}{R}[/latex].
The CO represents the blood being ejecting from the left ventricle into the aorta. If CO is decreased, less blood will be entering the aorta. Relating this scenario to the flow equation, a reduced CO means a decrease in P1, and since we are not yet discussing flow out of the compartment, P2 stays constant. A reduction in P1 decreases the overall pressure gradient, and Q (flow) is reduced. In contrast, an increase in CO will cause an increase in P1 as more blood will be entering the compartment (P1). Assuming pressure within the compartment remains constant (P2), this will cause an increase in the pressure gradient and therefore increased blood flow (Q).
Resistance arterioles influence the blood exiting the vessel. Resistance arterioles can increase or decrease the amount of blood permitted to leave the compartment through constricting or dilating. When discussing the mechanisms concerning the circulatory system, they are referred to as vasoconstriction and vasodilation. These terms are discussed in detail later in the subchapter. Constricting the resistance arterioles will reduce the vessel’s radius and less blood will leave the compartment. Dilating the resistance arterioles will expand the vessel’s radius and permit more blood to exit the compartment.
Mean Arterial Pressure as a Function of Cardiac Output and Total Peripheral Resistance
Using the logic above, we will now look at an equation that can relate these concepts to the entirety of the vasculature. MAP refers to the average arterial pressure in one cardiac cycle, and represents the pressure within the aortic compartment. TPR (total peripheral resistance) is the sum of the resistance in the body, and represents the resistance arterioles within the system. Applying these concepts allows us to estimate the sum of blood flow (Q) throughout the systemic circulation as the pressure within the aorta (MAP) will be controlled by CO and TPR as displayed below:
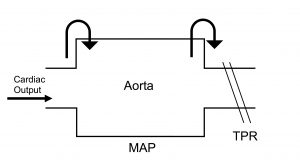
For example, if CO increases, MAP increases as more blood enters the aorta and pressure in the vessel increases. Whereas if TPR increases, MAP increases as less volume exits the compartment, increasing the pressure. Practice using this logic to infer MAP if CO or TPR were decreased.
Remember to keep the flow equation in mind when considering how the blood flow will increase or decrease. Always define what your P1 and P2 are in each situation.
Example: The aortic pressure is P1 in reference to resistance arterioles as P2. The aorta can be seen as P2 in reference to the hearts pressure (CO) as P1. DO NOT FORGET, changes in vasodilation and vasoconstriction affect resistance and not pressure.
Test Your Knowledge
Clinical Application:
Imagine you are a cardiologist treating a patient with diagnosed atherosclerosis. You know that atherosclerosis is a condition in which fatty deposits build up within the arteries causing the vessels to narrow and lose compliance. The patient reports feelings of cramping and pain in his limbs, and these symptoms become exacerbated with exercise. Explain why this makes sense. Hint: Think about the narrowing vessel’s resulting impact on the resistance to blood flow.
If this clinical example interests you, maybe a career as a cardiologist would too?
Vasodilation and Vasoconstriction
The nervous system can control the cardiovascular system by increasing or decreasing the radii of vasculature. This can be done through two opposing mechanisms. Vasodilation is the dilation of the vessel causing increased radii, thus increased blood flow. Whereas vasoconstriction is the constriction of the vessel causing decreased radii, thus decreased blood flow.
Test Your Knowledge
Clinical Application:
α1- adrenoceptor agonists, such as methoxamine and phenylephrine, are systemic vasoconstrictors prescribed to treat hypotension (low blood pressure). Explain how a medication designed to induce systemic vasoconstriction would be successful in combatting hypotension. Use the figure below to help explain your answer. Hint: Recall the effect vasoconstriction has on vessel radius and how this relationship would impact pressure in a compartment.
Factors Influencing Vasoconstriction
Vasoconstriction and vasodilation of vascular smooth muscle can be influenced by various factors such as; neural, autocrine, paracrine, and endocrine. Neural input refers to the innervation of all blood vessels, except for capillaries, by the Sympathetic Nervous System (SNS). Autocrine influence occurs through cells releasing compounds that stimulate the original cell. For example, cells can release the vasoactive compound NO (nitric oxide), which can vasodilate the cell that produced it. Paracrine influence includes the release of vasoactive compounds from surrounding tissue or endothelial cells. Finally, endocrine factors are stimulated by SNS activation in relation to the adrenal glands that will affect vascular smooth muscle based on the adrenergic membrane receptor population present on the tissues.
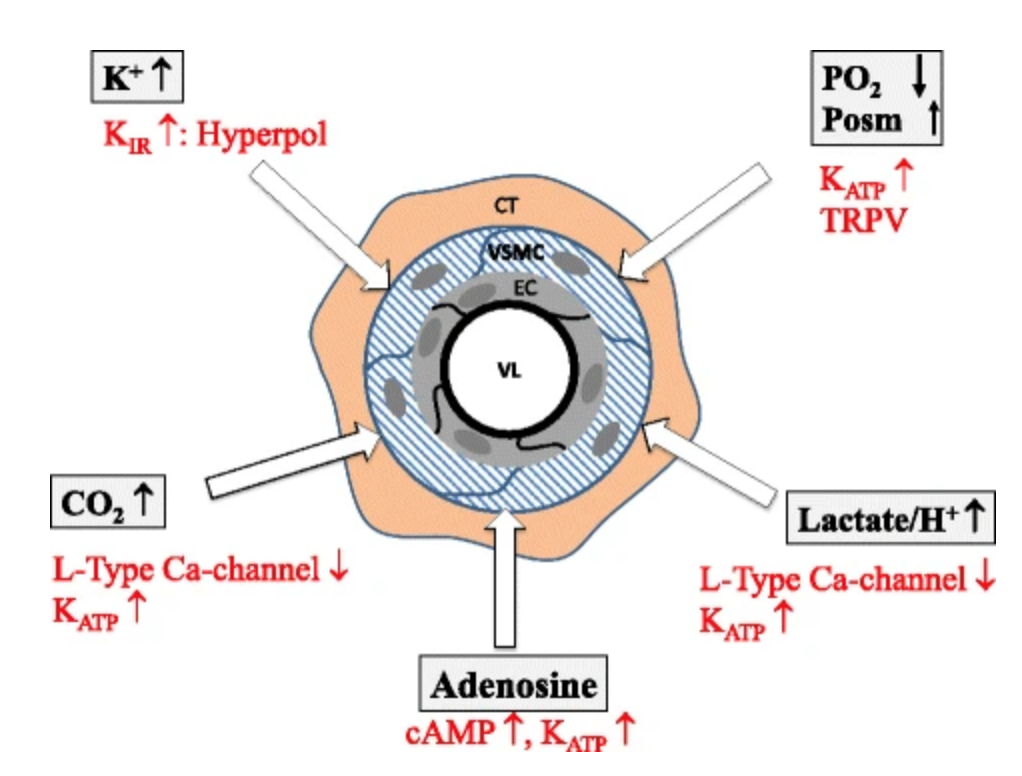
The following diagram is above course level but offers a few examples of the paracrine influence through local vasoconstrictors released due to tissue metabolic activity. A good way to understand this concept is to think about this concept in terms of exercise… going for a run will cause internal H+ (hydrogen ions) and CO2 (carbon dioxide) levels to increase.
Vasodilation Video
The following video offers a good explanation of the importance of the paracrine endothelial influence on blood pressure and describes NO as an example of a vasodilator. The video goes into more detail than needs to be understood for this course, but watching it over once and just listening will give a good idea of the main concepts of vasodilation.
Tips From Past Students
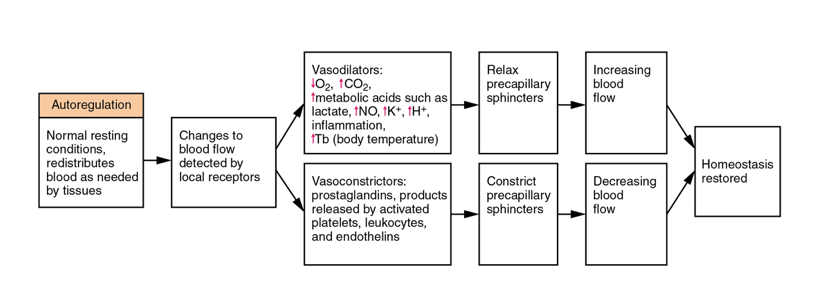
Apart from nervous system innervation, it is important to realize that vasodilation and vasoconstriction are simply opposite reactions of each other. If you understand this, the only part of the following flow chart that needs to be memorized is the third box describing the various vasoconstrictors and vasodilators.
Radius Control Flow Chart
The flow chart below offers a great summary of the subchapter in a way that is very intuitive. Under normal conditions, the vasoconstriction/ vasodilated status of vascular smooth muscle is maintained through auto-regulation. This helps to ensure that adequate blood is distributed to all body tissues. However, there are many situations in which blood flow will fluctuate beyond the limits of its homeostatic range. Local receptors will detect these increases or decreases and initiate the proper cascade to restore homeostasis. Try going through each step without looking at the chart. What would happen if local receptors detect high blood pressure? Or low blood pressure?
Test Your Knowledge
Thinking Beyond:
When exercising, the systemic circulation vasculature experiences a combination of vasoconstriction and vasodilation. Whether the blood vessel experiences vasoconstriction or vasodilation is tissue-dependent. What tissues would you expect to experience reduced blood flow due to vascular vasoconstriction? What tissues would you expect to experience enhanced blood flow due to vascular vasodilation? Hint: Consider what tissues would demand more oxygen when exercising.
What vasoactive compounds may be released by these tissues to signal the demand for increased blood flow? Hint: Paracrine regulation on vascular smooth muscle by-products of tissue metabolism.
Key Takeaways
Consider the following concepts to help guide your studies:
- The vascular components of the circulatory system yield variances in their structural compositions. The differences in the structural design of arteries, veins, and capillaries relate to the compartments’ function.
- Blood flow is dependent on pressure gradients and resistance of the system. This relationship is reflected in the following equation: [latex]Q = \frac{(P1 - P2)}{R}[/latex]
- Resistance of the circulatory system is inversely proportional to the vessel radius. Vasoconstriction refers to decreased vessel radius and therefore decreased flow, whereas vasodilation refers to an increase in vessel radius and therefore an increased flow.
Subchapter Quiz
The questions below can be used to assess your knowledge within this chapter. There are five multiple-choice questions that you should attempt without referring to your notes. The questions will provide you with responses to your answers to guide your studying but should not be used as your only resource.
Media Attributions
- Diagram of blood vessel structures © Begoon adapted by Begoon is licensed under a CC BY-SA (Attribution ShareAlike) license
- MAP Diagram 2 © Yonatan Fortinsky is licensed under a Public Domain license
- MAP Diagram © Yonatan Fortinsky is licensed under a Public Domain license
- Arteriole cross section © Matthias Jacob, Daniel Chappell, Bernhard F. Becker is licensed under a CC BY (Attribution) license
- Radius autoregulation flow chart © J. Gordon Betts, Kelly A. Young, James A. Wise, Eddie Johnson, Brandon Poe, Dean H. Kruse, Oksana Korol, Jody E. Johnson, Mark Womble, Peter DeSaix is licensed under a CC BY (Attribution) license
The arrangement of blood vessels within an organ or body part.
Contraction of smooth muscle cells and the tightening of blood vessels. This will allow for less blood flow through the vasculature.
Relaxation of smooth muscle cells and the widening of blood vessels. This will allow for more blood flow through the vasculature.
The opposite of stiffness. Describes how much an object will stretch when under a given force.

