Heart Anatomy & Circulatory System Blood Flow
The heart is built to efficiently fill, oxidize, and pump blood throughout the body. In order to do this, it requires chambers, valves, and electrical signals to properly accomplish its goals. This chapter also discusses the anatomy of the heart, which acts as a strong background for the the rest of the heart and vasculature unit.
Learning Outcomes
In this section you will learn…
- The general anatomical features of the heart that are important for contraction and blood flow.
- Why the heart is compartmentalized and how it facilitates function.
- The pathway of blood flow throughout the body.
Heart Anatomy
The heart is a composed of two pumps and two pipes. The closed-circuit design of the heart means that no variable is independent from the others. Whenever a variable, such as cardiac output (CO), is altered, it will affect the other variables. This is an important concept to understand as you continue through the units of this subchapter.
Tips From Past Students
When you are looking at a heart, remember it is in reference to anatomical position (the left and right of the specimen, not your own).
Specialized Conduction Components of the Heart
This diagram showcases the heart through the orientation of the frontal plane. The figure is labeled to showcase the heart’s basic anatomical structures, including; right and left atria and ventricles, and the aorta. The figure also highlights the specialized electrical conducting components such as; the sinoatrial (SA) node, atrioventricular (AV) node, bundle of His, and the Purkinje fibers. The white arrows illustrate the pathway of electrical conductance between these structures of the heart.
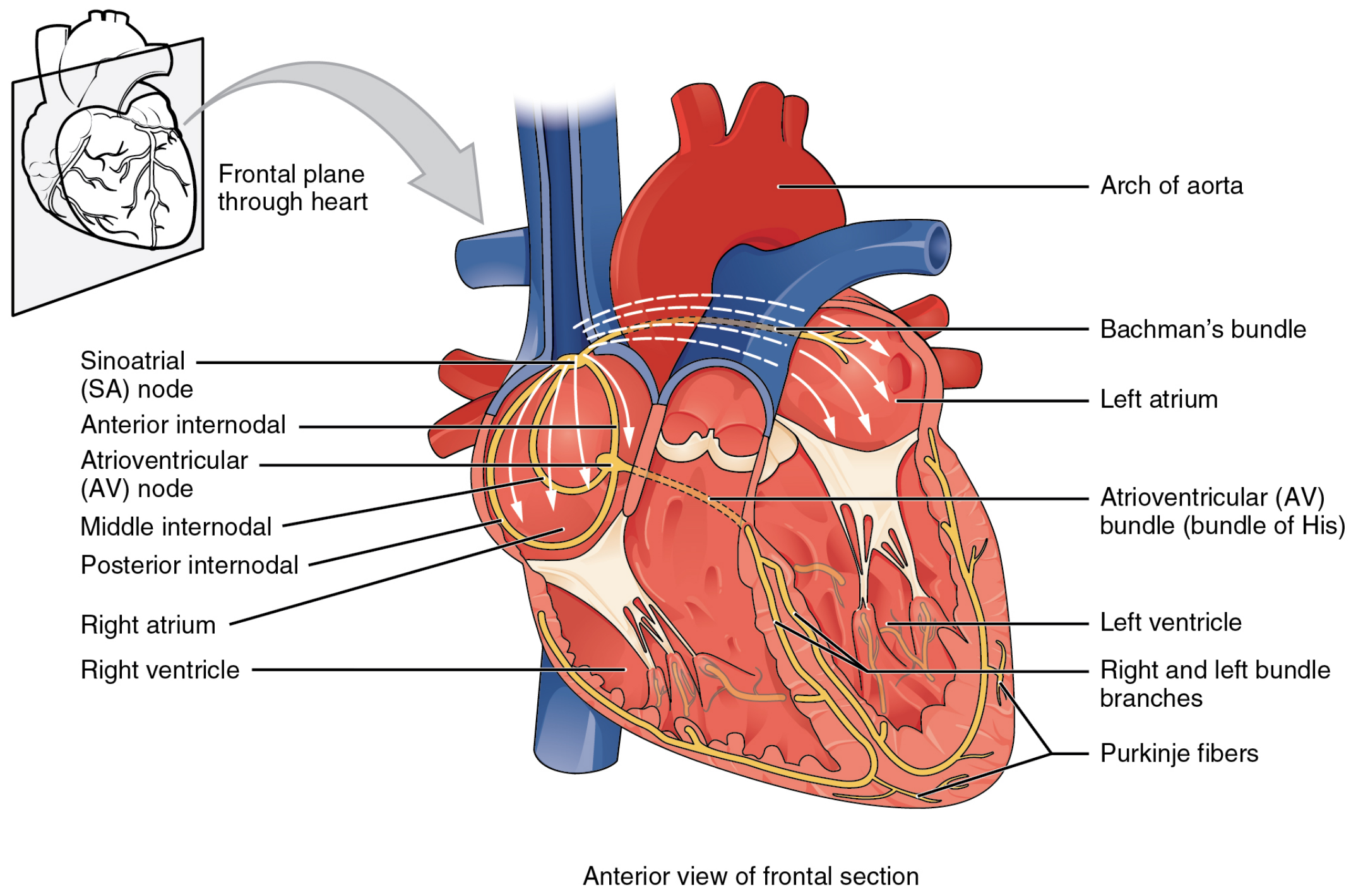
When looking at this diagram, take note that the left ventricle of the heart is much bigger and more muscular than the right because it has the hard job of pumping the oxygenated blood through the aorta to the rest of the body.
Test Your Knowledge
Thinking Beyond:
Describe the electrical pathway of depolarization in the heart. Why is this ordered pattern of depolarization important for coordinated contraction of the cardiac myocytes? Hint: Think about the significance the depolarization- contraction relationship has on proper blood flow.
Compartmentalization of the Circulatory System
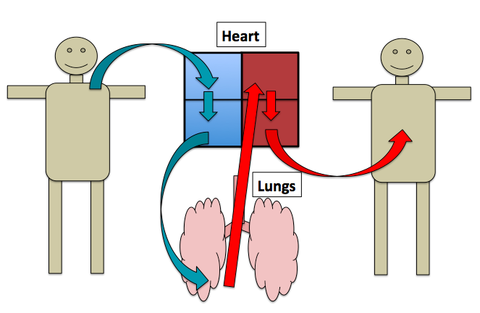
The heart is composed of two pumps and pipes. The two pumps that comprise the heart are the left heart and the right heart. These pumps present functionally different purposes. The left heart is responsible for pumping blood from the left ventricle and directing the flow to the tissues, otherwise referred to as systemic circulation. The right heart is responsible for pumping blood across the lungs, referred to as pulmonary circulation.
This figure was included because it shows the path of blood through the heart, body, and lungs on a macroscopic scale. This simplified schematic provides a visualization that may promote a better understanding. The diagram also does an excellent job of solidifying the idea that the left atria and left ventricle are functionally separate from the right atria and right ventricle. Though they can directly impact each other, they receive and send blood to different locations.
Functional Compartmentalization of the Heart
The figure below depicts functional compartmentalization of the human circulatory system which is a key topic to understand before learning details of this system. This section will help with understanding pressure differences and blood flow as it shows you where the structures are located.
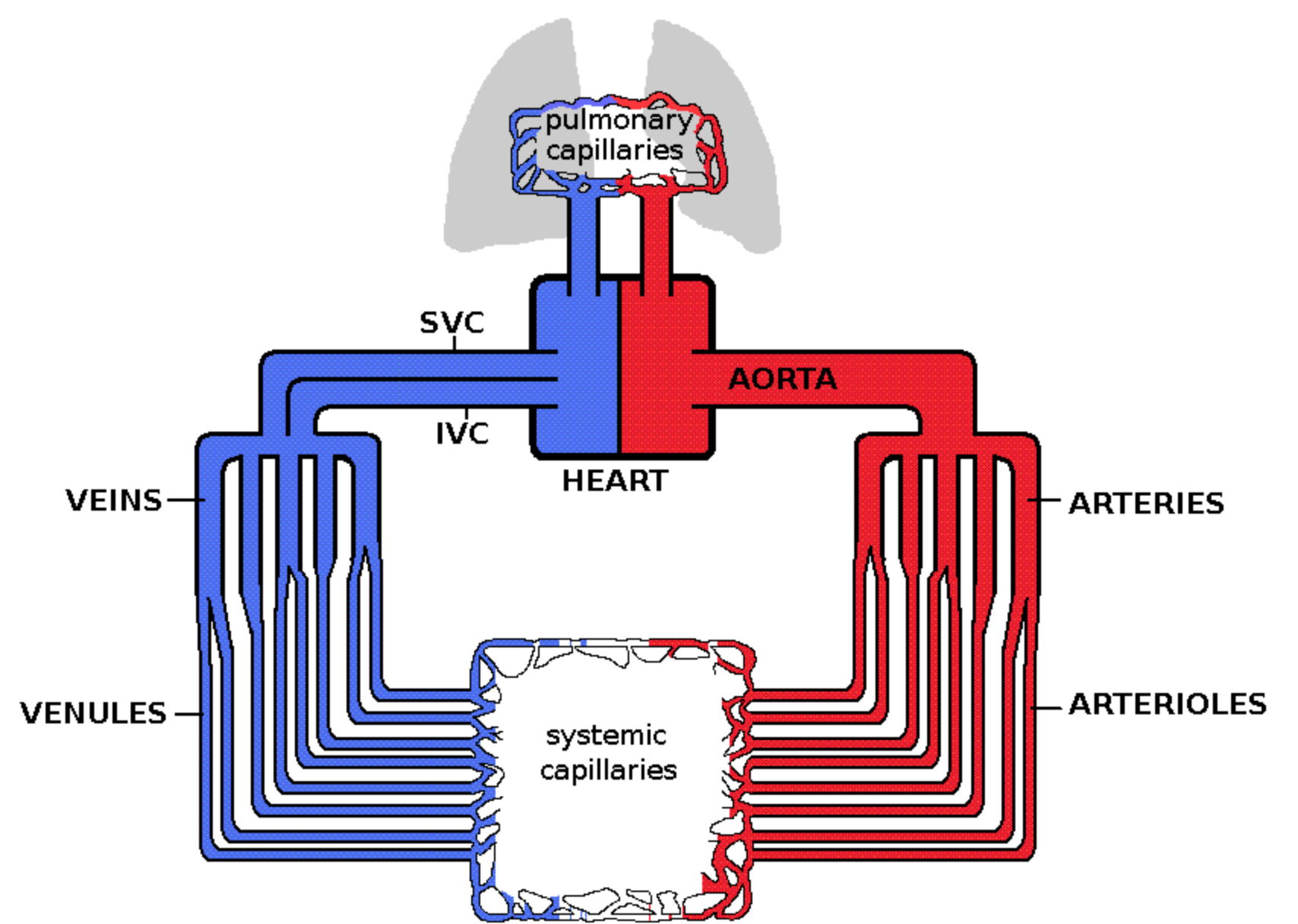
Read the diagram clockwise to follow the flow of blood.
Blood oxygenated via the pulmonary capillary bed leaves the heart through the aorta, then travels to the arteries, followed by the arterioles which lead to the systemic capillaries. Oxygen diffuses to the tissues, causing deoxygenated blood to travel back to the heart via the venules. These combine into veins, which drain into the superior and inferior vena cava, then to the right heart. The blood undergoes gas exchange at the pulmonary capillary bed and the cycle begins again.
Test Your Knowledge
Thinking Beyond:
Functional compartmentalization is used by many body systems – not just the circulatory system! In fact, we spoke about functional compartmentalization when discussing the gastrointestinal tract in HK*2810. Try to connect these systems by considering their differences and similarities. What relationship do compartments have with each other? How does this relationship influence the regulation of each system? Hint: Consider how these systems communicate at the cellular level to achieve their shared goal.
Comparison of Pulmonary and Systemic Capillaries
The capillary beds of the circulatory system serve the purpose of conducting gas exchange. In the systemic circulation, the capillaries allow for oxygen delivery into the body tissues. In the pulmonary circulation, the capillaries of the lungs allow for the O2 (oxygen) we breathe in to enter the bloodstream while CO2 (carbon dioxide) is removed.
The diagram below illustrates the relative locations of pulmonary capillaries, vasculature, compartments of the heart, and sites of gas exchange. The diagram can also be used to compare systemic and pulmonary capillaries. Notice how in the lung’s pulmonary capillaries, the O2 we inhale is added to the blood, and the CO2 is removed. The systemic capillaries showcase the reverse process as O2 is removed from the blood to be used by active tissues that produce CO2 as a byproduct.
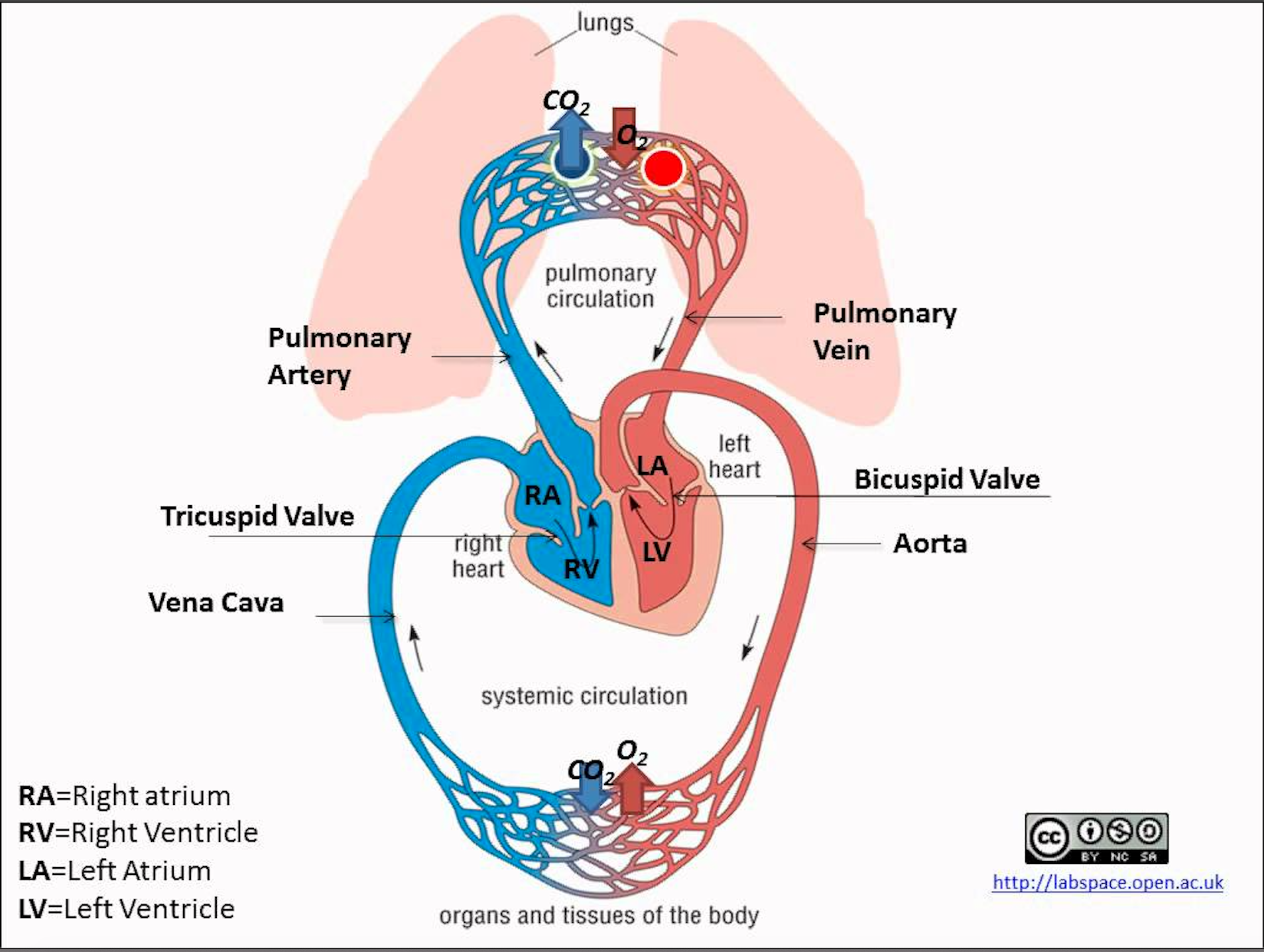
Both systems are composed of arterioles and venules. These arise from arteries and feed into veins. However, systemic capillaries are regulated by resistance arterioles to a greater degree than pulmonary capillaries. This is so that fluctuations in resistance do not affect oxygenation at the lung. We will talk more about resistance later in this section. The big thing to take away from here is that pulmonary and systemic capillaries are set up in the same way but are regulated differently.
Test Your Knowledge
Clinical Application:
In order to determine whether someone is having a left or a right heart attack, doctors will check the systemic and pulmonary compartments for fluid build-up:
- A RIGHT heart attack = fluid build up in the peripheral tissues.
- A LEFT heart attack = fluid build up in the lungs.
Using what you’ve just learned about heart anatomy and the direction of blood flow in the circulatory system, explain why this is true. Hint: Think about the pathway of blood after going through the right heart vs. the left heart.
If this clinical example interests you, maybe a career as a cardiologist would too?
Blood Flow
Pathway of Blood Flow
Now that you understand how the heart and the circulatory system are organized, we can examine the pathway of blood in closer detail.
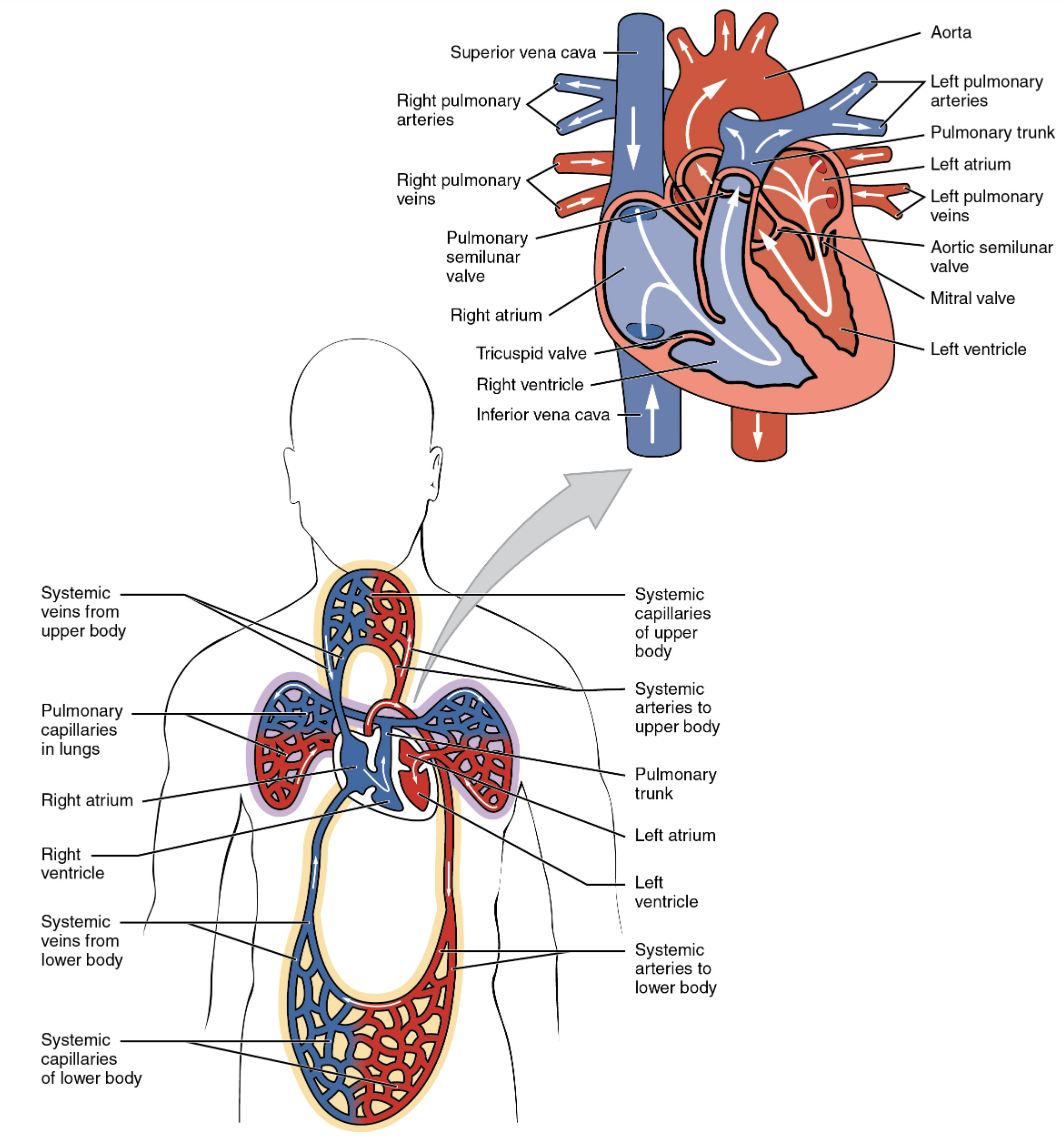
Blood flows from the right atrium to the right ventricle, where it is pumped into the pulmonary circuit. The blood in the pulmonary artery branches is low in O2 but relatively high in CO2. Gas exchange occurs in the pulmonary capillaries (O2 into the blood, CO2 out), and blood high in O2 and low in CO2 is returned to the left atrium. From here, blood enters the left ventricle, which pumps it into the systemic circuit. Following the exchange in the systemic capillaries (O2 and nutrients out of the capillaries and CO2 and wastes in), blood returns to the right atrium, and the cycle is repeated.
Tips From Past Students
An easy way to memorize the direction of blood flow…
- Arteries carry blood Away from the heart, where as veins carry blood back towards the heart.
Valves of the Heart
The heart’s anatomical structure includes the presence of four valves that function to promote proper blood flow through the organ. Two of the four valves are referred to as atrioventricular valves, including the tricuspid valve located between the right atria and ventricle and the mitral valve located between the left atria and ventricle. The other two valves include; the pulmonary valve located between the right ventricle and the pulmonary arteries and the aortic valve located between the left ventricle and the aorta. All the valves are passive as their opening and closing are controlled by pressure gradients. Contraction of the right atria causes the pressure within the atria to become greater than the pressure in the right ventricle. This opens the tricuspid valve, and blood flows from the right atria to the ventricle. As blood fills the right ventricle, pressure builds, followed by the contraction of the right ventricle. This closes the tricuspid valve and opens the pulmonary valve, permitting blood flow across the lungs. Oxygenated blood returns to the heart through the pulmonary veins and into the left atria, which contracts to open the mitral valve. Blood flows from the left atria to the left ventricle through the mitral valve. Finally, as the left ventricle fills, pressure builds, and the ventricle begins to contract. This causes the closure of the mitral valve and the opening of the aortic valve, facilitating blood flow out of the heart and into the systemic circulation. Proper functionality of these valves is critical for the heart’s efficiency as passage through the valves ensures the adequate filling of the chambers while the closure of the valves prevents back-flow. Refer to figure 5 for a visual representation of these chambers within the structure of the heart.
Test Your Knowledge
Real-Life Scenario:
The fossa ovalis is a small region in the interatrial septum (the wall of muscle separating the left and right atria). Prior to birth, this region remains an open hole known as the foramen ovalis which allows blood flow between the right and left heart. In utero, this hole remains open because blood flow is not required across lungs since the fetus is receiving oxygen through the placenta. However, once born, the fetus will utilize their lungs to receive oxygen and the foramen ovalis will close forming the fossa ovalis. What would happen to the heart if this hole did not close?[1] Hint: Think about the flow of blood in the right heart in contrast to the left heart. If this hole failed to close, the two circulations would not be separated.
For more information and the answer to this question, read this short article.
Key Takeaways
Consider the following concepts to help guide your studies:
- The anatomy of the heart and circulatory system is essentially composed of two “pumps” ; the right heart and left heart, and various connective “pipes” ; arteries, veins, and capillaries.
- Blood flows throughout the closed circuit of the circulatory system following the path of; left ventricle → aorta → systemic arteries → systemic capillaries → systemic veins → superior and inferior vena cava → right atrium → right ventricle → pulmonary arteries → pulmonary capillaries → pulmonary veins → left ventricle.
- The systemic circulation is responsible for delivering oxygenated blood to the body tissues, whereas the pulmonary circulation is responsible for blood flow across the lungs.
- Capillary beds facilitate the function of gas exchange. The systemic capillary beds conduct gas exchange supplying oxygen to the tissues. The pulmonary capillary beds conduct gas exchange where new oxygen inhaled is exchanged for carbon dioxide we exhale.
Subchapter Quiz
The questions below can be used to assess your knowledge within this chapter. There are five multiple-choice questions that you should attempt without referring to your notes. The questions will provide you with responses to your answers to guide your studying but should not be used as your only resource.
Media Attributions
- Conduction System of Heart © J. Gordon Betts, Kelly A. Young, James A. Wise, Eddie Johnson, Brandon Poe, Dean H. Kruse, Oksana Korol, Jody E. Johnson, Mark Womble, Peter DeSaix is licensed under a CC BY (Attribution) license
- The Heart is a Double Pump © Khan Academy is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- Diagram of human circulatory system © Gccwang is licensed under a CC BY-SA (Attribution ShareAlike) license
- What is the difference between pulmonary and systemic circulations? © JohnsonZ. Mandira P. is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- Dual system of the Human Blood Circulation © J. Gordon Betts, Kelly A. Young, James A. Wise, Eddie Johnson, Brandon Poe, Dean H. Kruse, Oksana Korol, Jody E. Johnson, Mark Womble, Peter DeSaix is licensed under a CC BY (Attribution) license
- Giblett, J.P., Abdul-Samad, O., Shapiro, L.M., Rana, B.S., Calvert, P.A.(2019). Patent Foramen Ovale Closure in 2019. Interv Cardiol, 14(1), 34-41. http://doi.org/10.15420/icr.2018.33.2 ↵
A standard orientation with the body upright and hands by sides.
Large lower compartment of the heart which pumps blood out to the body.
The breakdown of a system into smaller more detailed sections or "compartments" that all work together to produce one main outcome or "function".
Vessel that carry oxygen-rich blood away from the heart.
Smaller vessel that branches off of arteries, moving blood to capillary beds.
Small blood vessel that allows blood to flow from capillary beds to veins.
Vessels that bring oxygen depleted blood back to the heart.
Smaller upper compartments of the heart which empty blood into the ventricles.