Glomerular Filtration
Glomerular filtration is a key step in the production of urine and is an important topic as it impacts the future actions of the kidney. It is regulated by hormones, autoregulation and the nervous system. GFR, or glomerular filtration rate, will be discussed in depth throughout this subchapter.
Learning Outcomes
In this section you will learn…
- Explain how the kidney filters the blood to produce urine.
- Understand the glomerular filtration rate (GFR), including the hydrostatic and osmotic forces that favour and oppose filtration.
- Describe the mechanisms that regulate glomerular filtration rate.
- Regulation of renal blood flow and capillary hydrostatic pressure.
- Autonomic regulation of GFR.
- Physiological regulation of GFR.
- Auto-regulation, tubuloglomerular feedback, and the myogenic response of the kidney.
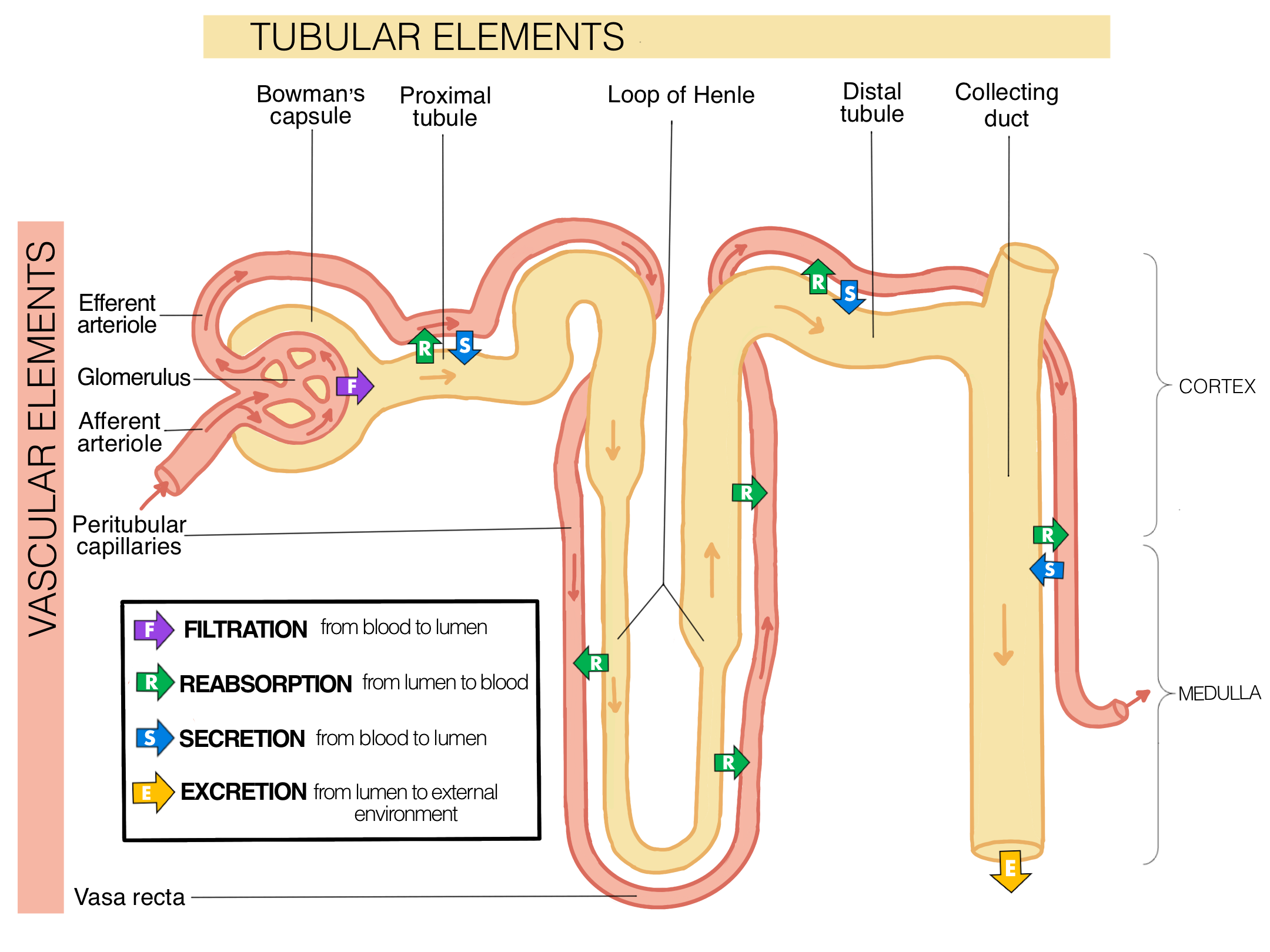
This diagram depicts an overview of fluid flux between the vasculature system and the tubular system of the nephron in the kidney. This diagram is similar to the one found in the course notes and gives a broad overview of the topics we are about to discuss in more detail.
Tips From Past Students
Keep in mind that everything is filtered from the blood in the glomerulus into the tube at Bowman’s capsule then the kidney works to reabsorb the important things back into the blood and everything else is eliminated from the body as urine (don’t worry you will learn more about this soon!).
Filtration
The process of producing urine involves; filtration, reabsoprtion, secretion and excretion, with the goal to eliminate waste in the form of urine. Take note in the diagram above where each of these processed occur along the nephron and collecting ducts.
The formation of urine begins with the process of filtration.
Filtration occurs at the filtration membrane, which is located at the boundary between the glomerulus and the Bowman’s capsule. The filtration membrane permits the rapid movement of filtrate from the capillary bed to the capsule. The fenestrations that are found in the glomerulus and the podocyte filtration slits prevent the filtration of blood cells or large proteins while allowing most constituents to pass through. Recall that the glomerulus exists between the afferent and efferent arterioles.
The filtrate is produced when in the high-pressure glomerulus; plasma components are driven through the filtration membrane and collect in the Bowman’s capsule. The non-filterable components (cells, serum albumins) will move through the glomerulus and exit via the efferent arteriole. The resulting filtrate is a dilute solution that includes water, electrolytes, wastes, nutrients, and other molecules that are able to pass through the membrane. It is important to note that many of these materials are reabsorbed through various parts of the nephron. The components filtered out of the capillary that are not reabsorbed will be excreted from the body.
Tips from past students
The function of the glomerulus is to filter everything out. This is a protective mechanism, as the body is unable to predict if toxic substances are taken in.
The function of the proximal tubule and the Loop of Henle is to take back the substances that the body needs (such as water and salt). Everything that is not reabsorbed will be excreted.
Did you know the electric charge is a factor that affects the ability of a substance to cross the filtration membrane? The proteins associated with podocytes and the basement membrane are negatively charged, so they tend to repel negatively charged substances, and allow positively charged substances to pass more freely. [1]
Glomerular Filtration Rate (GFR)
Ever wonder how much filtrate is returned to circulation via reabsorption? About 99% of the filtrate is returned so that only 1-2 L of urine is produced/day!
Did you know that men and women produce different amounts of filtrate each day? The kidney of men produce 180L/day of filtrate and women produce 150L/day
Filtration occurs as the pressure causes fluid and solutes through a semipermeable barrier with the solute movement constrained by particle size. Hydrostatic pressure is the pressure produced by a fluid against a surface. If you have fluid on both sides of a barrier and both fluids exert pressure in opposing directions, the net fluid movement will be in the direction of the lower pressure (solutes move from an area of high to low pressure).
Osmosis is the net movement of water across a semipermeable membrane. This creates an oncotic pressure. This pressure will exist until the solute concentration is the same on both sides of the semipermeable membrane. Water will only cross the membrane when solute concentrations on both sides of the membranes differ. The water moves from the side of the membrane with a low solute concentration to the side with a high solute concentration.
GFR represents the volume of filtrate formed by both kidneys per minute. The GFR is influenced by both the hydrostatic pressure and the colloid osmotic pressure (oncotic pressure) on either side of the capillary membrane of the glomerulus. Glomerular filtration will occur when the glomerular hydrostatic pressure exceeds the luminal hydrostatic pressure of the Bowman’s capsule. Thus, the net fluid movement will be into the Bowman’s capsule. There is also an opposing force, the oncotic pressure, which is typically higher in the glomerular capillary.
The osmotic pressure is exerted by the solutes inside the lumen of the capillary, as well as within the Bowman’s capsule. Since the filtration membrane limits the size of particles crossing the membrane, the osmotic pressure is higher in the capillary than in the Bowman’s capsule. [2]
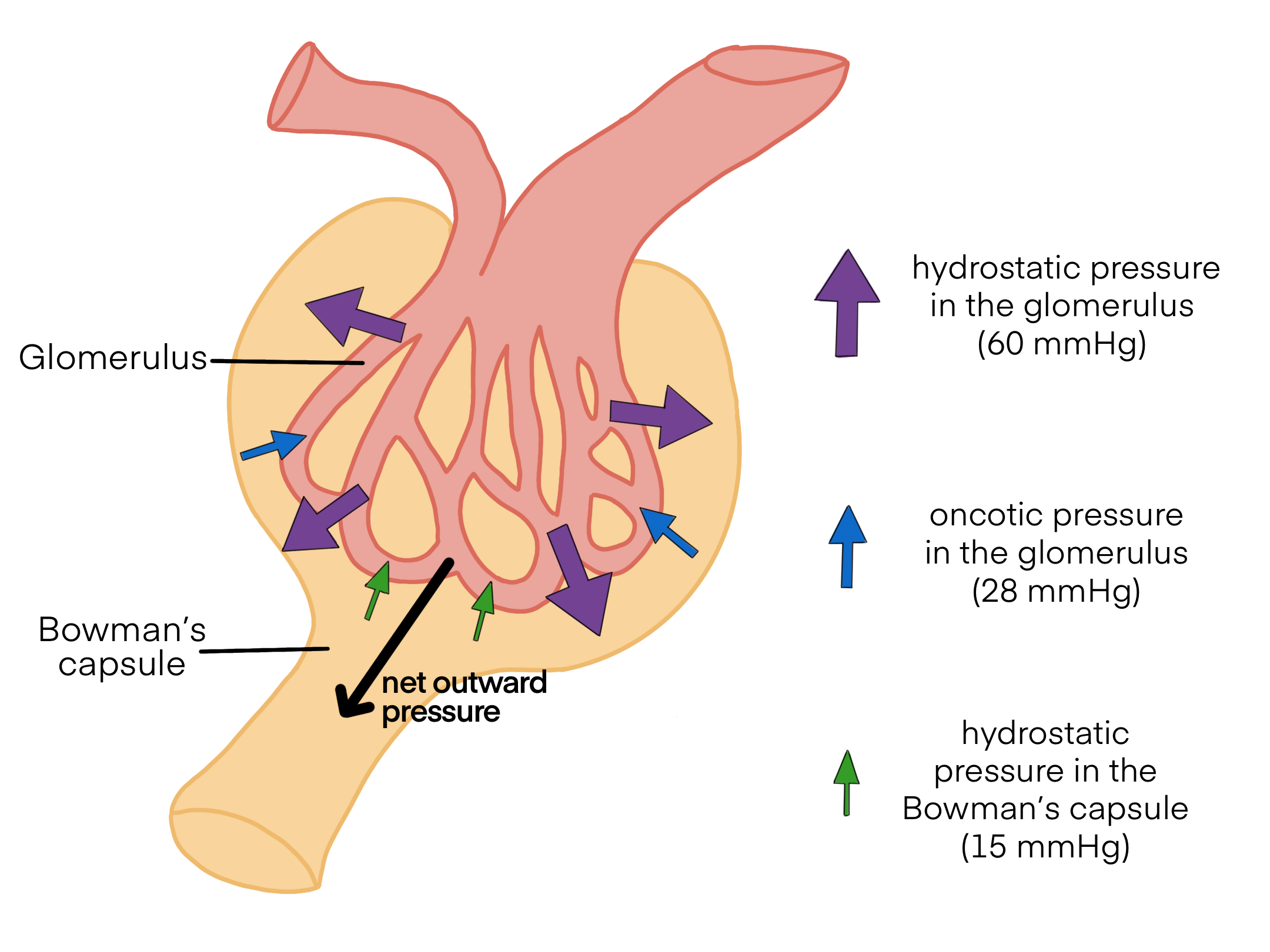
The figure below shows a schematic of the net filtration pressure. Understanding hydrostatic and oncotic pressure will help you grasp the concept of why solutes move in a certain direction.

The average osmotic pressure is 30mmHg within the capillary. The presence of proteins in the Bowman’s capsule results in an osmotic pressure that is ~0 mmHg; thus, only the pressure of fluid moving across the capillary into the Bowman’s capsule causes the hydrostatic pressure. The hydrostatic pressure is sufficient to push water through the membrane despite the oncotic pressure working against it. [3]
GFR Equation
GFR is the rate at which the kidneys filter blood. Recall that GFR at the level of the kidney is dependent on 4 variables: hydrostatic and osmotic pressure in the glomerulus and hydrostatic and osmotic pressure in Bowman’s capsule. The relationship between these variables is defined in a different GFR equation than we previously discussed. Kf represents the filtration coefficient which is a constant. PG is the hydrostatic pressure (~60mmHg) in the glomerulus and PBC is the hydrostatic pressure of the bowman’s capsule (~15mmHg). πG is the osmotic pressure of the glomerulus (~28mmHg) and πBC is the osmotic pressure of the Bowman’s capsule (~8mmHg).
[latex]GFR=K_f (({P_G - P_{BC}})-({\pi_G - \pi_{BC}}))[/latex]
This equation may seem overwhelming, but let’s work through the variables to understand how filtration occurs:
The blood inside the glomerulus creates a hydrostatic pressure of 60mmHg (PG), which is the force to move fluid out of the glomerulus into the lumen of Bowman’s capsule. The fluid in the Bowman’s capsule creates a hydrostatic pressure of 15 mmHg (PBC), which is the force to move fluid out of the Bowman’s capsule back into the glomerulus. Since there is a drop in pressure across the glomerular capillary bed (PG is greater than PBC), fluid will move in the direction of the lower pressure, so fluid will flow from the glomerulus into the Bowman’s capsule (which is filtration).
There is also an opposing force, the osmotic pressure. The osmotic pressure acting to draw water from the Bowman’s capsule into the glomerulus is 28mmHg (PBC). The absence of proteins within Bowman’s capsule results in a low osmotic pressure of 8mmHg (πBC).
Filtration across the whole glomerular capillary bed occurs because the difference between the hydrostatic pressure (PG – PBC) is greater than the difference between the osmotic pressure (πG – πBC). As you can see in the figure, the net movement of fluid is from the glomerulus to the Bowman’s capsule, which is filtration.
This diagram gives a visual representation of the variables in the GFR equation discussed above. The coloured arrows represent the different pressures and which way they are acting to move fluid. The larger the arrow indicates a larger pressure, thus, a greater force to move fluid in that direction. The absence of proteins within Bowman’s capsule results in osmotic pressure of 8mmHg, which is near zero, thus has little effect on the movement of fluid (which is why it is not on this diagram).
Did you know the GFR is roughly proportional to the metabolic body mass? This means larger animals have a bigger GFR!
Ever wonder how the GFR can be used to assess kidney function? GFR can be estimated by intravenous administration of insulin. Insulin is neither reabsorbed or secreted by the kidney. Therefore, its appearance in the urine is directly proportional to the rate at which it is filtered by the renal corpuscle. [4]
Net Filtration Pressure (NFP) Equation
The sum of all influences (osmotic and hydrostatic pressure) results in an NFP of about 10mmHg. This can be found using the NFP equation with HPG representing hydrostatic pressure in the glomerulus (~50-60mmHg), HPBC being the hydrostatic pressure of the Bowman’s capsule (~15mmHg) and OPG representing the oncotic pressure of the glomerulus (~30mmHg).
[latex]NFP=HP_G - ({HP_{BC} + OP_G})[/latex]
Minor changes in the osmolality of the blood can result in major changes in the amount of filtrate formed. If blood pressure is changed, the Glomerular capillary hydrostatic pressure will also change, impacting the overall NFP.
If the NFP is negative the fluid will move out of the capillary and into the interstitial fluid. This can have a number of important physiological implications.
The following video describes the connection between Net Filtration Pressure (NFP) and Glomerular Filtration Rate (GFR), and introduces the Filtration coefficient. The video also touches on hydrostatic pressure, and oncotic pressures, two concepts that were previously mentioned.
Tips From Past Students
We do not talk about the NFP equation in class so do not focus on memorizing this, it is here to reinforce the idea that the net filtration pressure results in the movement of fluid from the glomerulus into the Bowman’s capsule.
The GFR equation is more relevant to class so spend extra time being comfortable with this equation and understanding how the variables influence filtration at the glomerulus.
Regulation of the GFR
There are two major forces opposing GFR. These are the hydrostatic pressure in the Bowman’s space and the plasma protein osmotic pressure. These are not under physiological control. The filtration coefficient is also beyond the realms of physiological control.
On the other hand, the hydrostatic pressure in the capillaries and the renal blood flow are under physiological regulation and adjust filtration according to the needs of the body.
Renal Blood Flow Regulation & Hydrostatic Pressure
Sometimes it can be difficult to conceptualize hydrostatic pressure, oncotic and osmotic pressure, etc. This figure is useful in depicting how these various pressure influences the movement of filtrate through the capillaries.
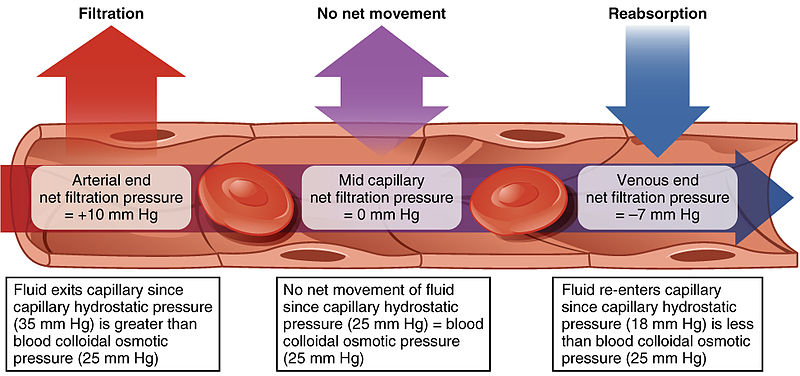
The above diagram shows the movement of fluid through the capillaries. It begins by showing the movement of fluid during filtration and it explains the hydrostatic and osmotic pressures required for filtration to occur. If there is no pressure difference there will be no net fluid movement. The reabsorption process occurs due to osmotic pressure being higher than hydrostatic pressure.
Renal blood flow and capillary hydrostatic pressure are determined by the arterial blood pressure coupled with the contraction of both the afferent and efferent arterioles. The total resistance of the afferent and efferent arterioles which is influenced by their degree of contraction determines the renal blood flow and any particular arterial pressure. Therefore, it is important that they change with arterial pressure in order to maintain a steady renal blood flow
Normally the afferent arteriole has a larger diameter than the efferent arteriole. This means that there is high resistance as the blood is forced from a wider vessel to a narrower one, this promotes filtration. If the arterial blood pressure remains constant then contracting the afferent or efferent vessels reduces blood flow and increases resistance. However, contracting either vessel has the opposite effect on the filtration pressure. If you contract the afferent arteriole there will be less of a pressure difference between the afferent and efferent arteriole; therefore, there will be a reduced filtration pressure. This will also decrease the amount of fluid that is able to pass from the afferent to efferent arterioles. However, if you constrict the efferent arteriole there is a greater pressure difference between the two vessels and the filtration pressure increases, and fluid becomes stuck between the afferent and efferent arterioles.
Overall, the constriction of the afferent arteriole decreases both blood flow and filtration pressure. Whereas, the constriction of the efferent arteriole decreases blood flow and increases filtration pressure (Both of these statements are assuming a constant blood pressure). The fact that the resistance of both the afferent and efferent arterioles can be altered allows for the independent regulation of GFR and blood flow.
Furthermore, capillary permeability can be increased by the release of certain cytokines, anaphylatoxins, or other mediators (such as leukotrienes, prostaglandins, histamine, bradykinin, etc.). These cytokines and mediators are released by cells during a state of inflammation. The NFP equation can be used to determine the net flux across the semipermeable membrane of the capillaries. [7]
Autonomic Regulation of GFR
Tips From Past Students
The kidneys are innervated by the sympathetic nerves of the autonomic nervous system.
- Sympathetic nervous activity – decreases blood flow to the kidney, making more blood available to other areas of the body during times of stress.
- The arteriolar myogenic mechanism – maintains a steady blood flow by causing the arteriolar smooth muscle to contract when blood pressure increases and causing it to relax when blood pressure decreases.
- Tubuloglomerular feedback – involves paracrine signaling at the JGA to cause vasoconstriction or vasodilation to maintain a steady rate of blood flow.
Remember that filtration removes solutes from the bloodstream, and will decrease blood flow
The kidneys are controlled autonomically by the sympathetic nervous system via the celiac plexus and the splenic nerves. A reduction of sympathetic stimulation results in vasodilation as well as increased blood flow through the kidney during resting conditions. Therefore, and increase in sympathetic stimulation leads to vasoconstriction and decreased flow.
Furthermore, when the frequency of the action potential increases, the arteriolar smooth muscle constricts (vasoconstriction); resulting in diminished glomerular flow, leading to a decrease in filtration due to a decreased flow.
Under conditions of stress, sympathetic nervous system activity increases, resulting in the direct vasoconstriction of afferent arterioles (norepinephrine effect) as well as the stimulation of the adrenal medulla. The adrenal medulla then produces generalized vasoconstriction through the release of epinephrine. This includes vasoconstriction of the afferent arterioles, further reducing the volume of blood flowing through the kidneys. This process redirects blood flow to other organs with more immediate requirements.
If blood pressure falls, the sympathetic nervous system will also stimulate the release of renin. This increases the production of powerful vasoconstrictors such as angiotensin II. Angiotensin II then stimulates aldosterone production, which will increase blood volume by reabsorption of Na+, resulting in increased water reabsorption.
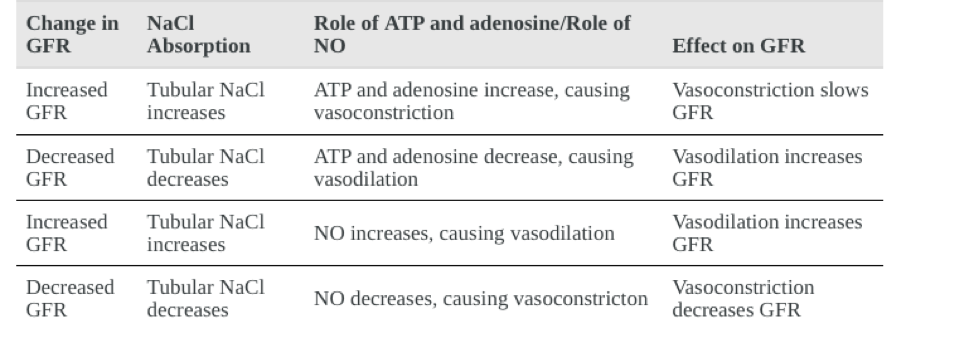
ATP and adenosine act locally as paracrine factors to stimulate the myogenic juxtaglomerular cells of the afferent arteriole to constrict, this slows blood flow and reduces GFR. [8]
A 10mmHg pressure differential is required across the glomerulus to maintain a normal GFR. Very small changes in arterial pressure significantly increases or decreases GFR.
As GFR increases there is less time for NaCl to be reabsorbed in the PCT (Proximal Convoluted Tubule), resulting in higher osmolarity in the filtrate. This increased osmolarity of the forming urine, and the greater flow rate within the DCT, activates the macula densa cells to respond by releasing ATP and adenosine (a metabolite of ATP).
When GFR decreases less Na+ is in the forming urine, and most will be reabsorbed before reaching the macula densa, which will result in decreased ATP and adenosine, allowing the afferent arteriole to dilate and increase GFR. NO has the opposite effect, relaxing the afferent arteriole, at the same time ATP and adenosine are stimulating it to contract. Thus, NO fine-tunes the effects of adenosine and ATP on GFR. [9]
This chart shows the Paracrine impacts on GFR, how they are achieved and the end result of this initial change. This is a good reference as you are going through your notes and studying.
Physiological Regulation of GFR
The main physiological systems which regulate renal blood flow and GFR are autoregulation, the myogenic response and tubuloglomerular feedback (TGF). These processes regulate blood flow over a range of blood pressures, such as when blood pressure decreases in sleep and increases while exercising.
In order for the kidneys to optimally function to maintain homeostasis in the body, it is essential that there are few changes to the glomerular filtration rate (GFR).
A possible problem occurs if there is an increase in GFR, such as from having increased blood volume and pressure, this will increase the volume and rate of fluid that flows through the proximal tubule but decrease the time this fluid is able to spend in the tube, known as equilibration time. A decrease in equilibration time reduces the amount of time for solutes to be reabsorbed back into the blood at the proximal tubule. This will result in the important solutes remaining in the tube of the nephron and be lost through excretion, which is a major problem. Thus, GFR must be regulated.
GFR is tightly and locally regulated at the kidney by three mechanisms:
- Autoregulation (myogenic response)
- Tubuloglomerular feedback
- Renin
Autoregulation
Recall our discussion about autoregulation used to regulate the kidney vasculature previously in this chapter. In this same way, autoregulation is used to regulate GFR.
[latex]Q=\frac{P_A-P_E}{R}[/latex]
The figure below represents a graphical depiction of the mechanism of autoregulation. Notice that as MAP increases (on the x-axis), GFR will remain constant over a range of pressures of ~80 to 160 mmHg (on the y-axis).
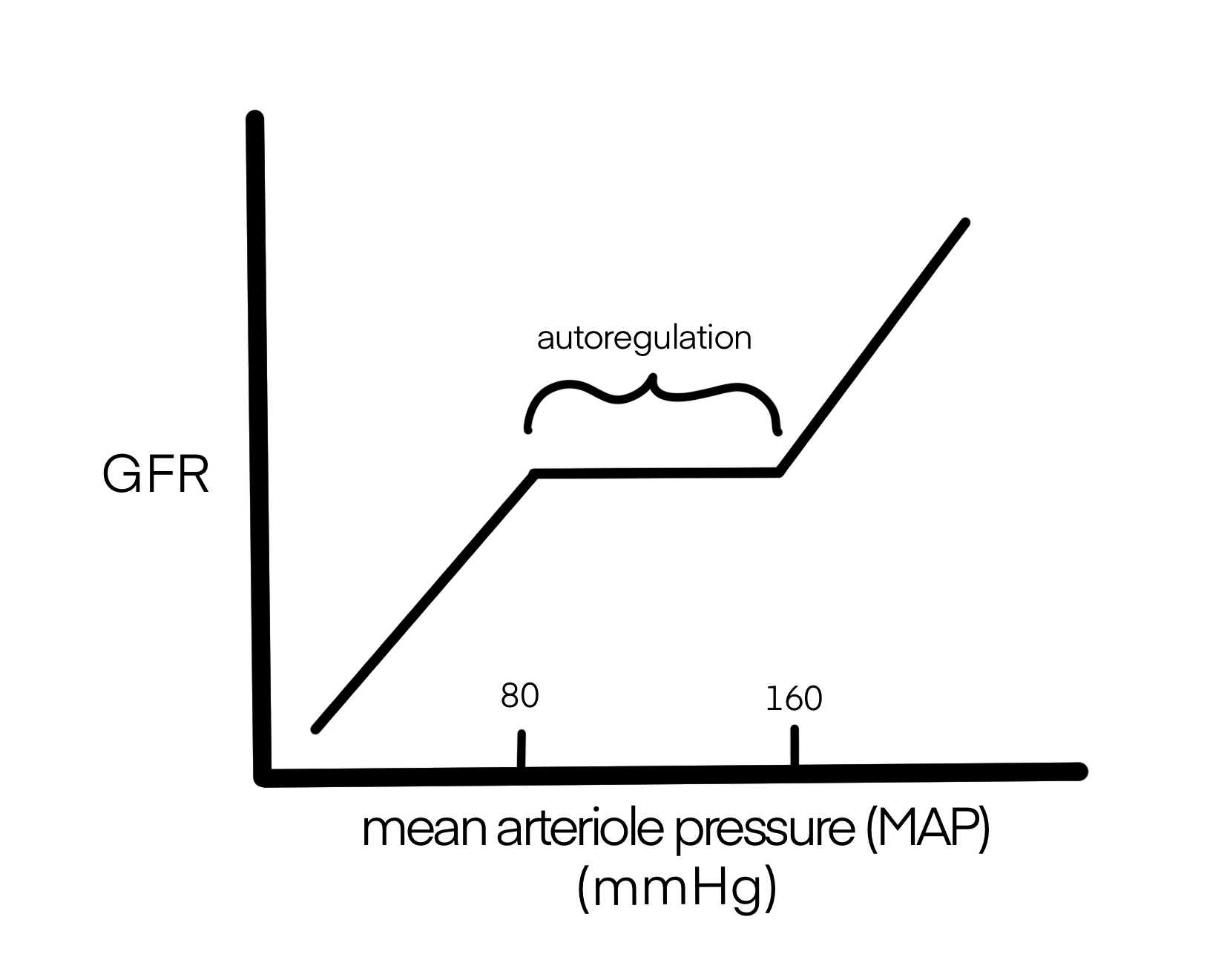
Figure 6. Autoregulation keeps GFR constant over a range of mean arteriole pressures.
The Limitations of Autoregulation
Despite the efforts of the autoregulatory system, an increase in blood pressure will still lead to a small increase in the secretion of salt and water. Even a small percentage change in GFR leads to a large percentage change in the excretion of salt and water. However, this excretion is less drastic than it would be without autoregulation. Furthermore, autoregulation helps restore the pressure to normal. This increase in urinary output as a result of an increase in arterial blood pressure is termed pressure diuresis. [10]
Myogenic Response:
In the kidney, the myogenic response ensures filtration rate (GFR) remains constant over a range of mean arterial pressures (MAP). This ensures that reabsorption in the proximal tubule remains constant so that important solutes are not lost from the body. Recall that an increase in pressure in the afferent arteriole will cause stretching of the vascular smooth muscle, leading to contraction of the smooth muscle in the afferent arteriole. This prevents increases in RBF (Q) and GFR that would damage the kidney.
The diagram below gives a visual representation of the myogenic response. Take note of how an increase in RBF causes stretching of the smooth muscle in the afferent arterioles. This results in contraction, or vasoconstriction, to decrease RBF and GFR, thus keeping them constant despite changes in pressure.
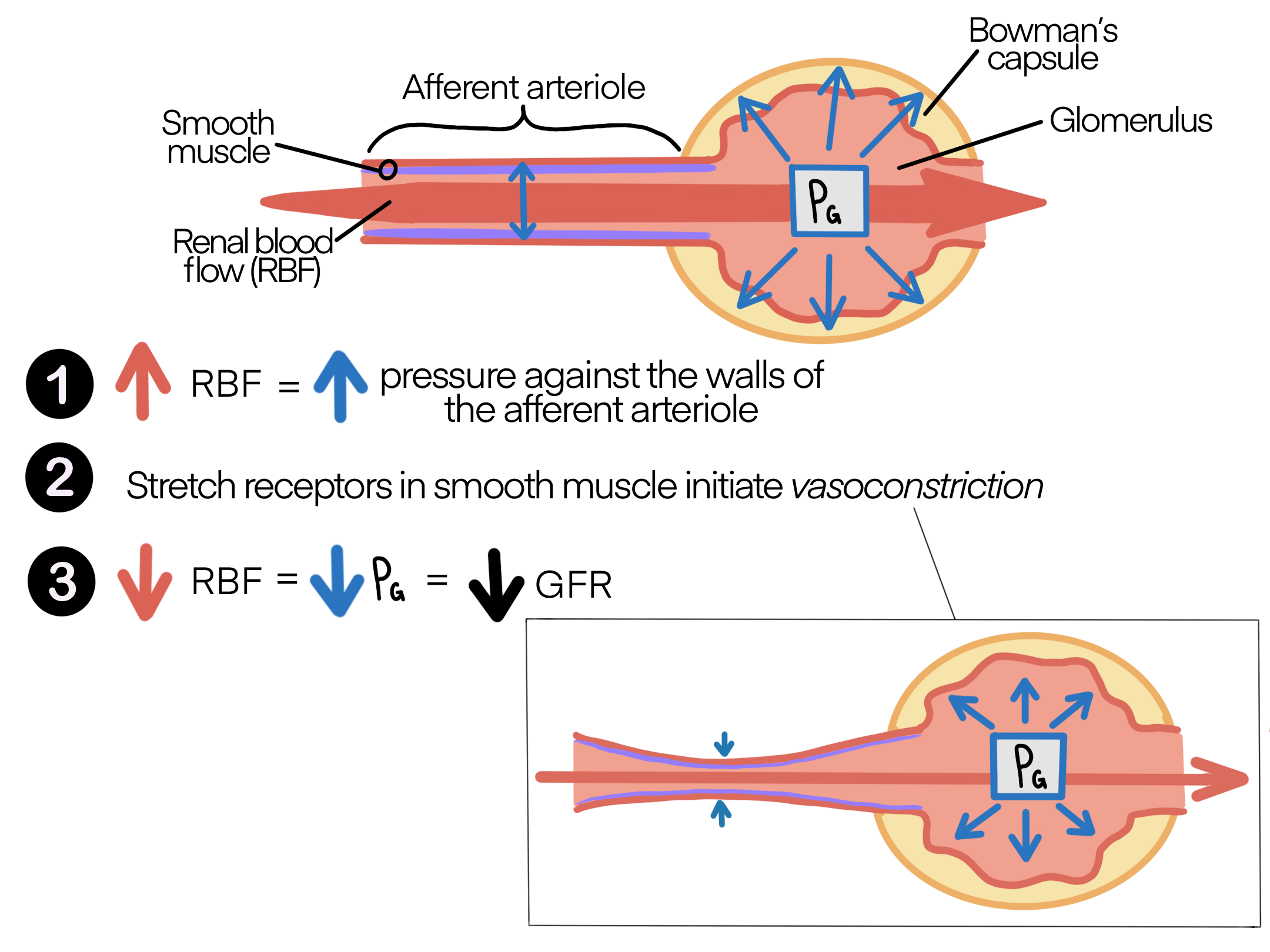
Stretching of blood vessels due to increased blood volume causes the blood vessel to rapidly decrease their diameter; pushing against the increased volume within the vessel. This results in increased resistance to blood flow and thus keeping the GFR constant. [11]
Tubuloglomerular Feedback (TGF):
The tubuloglomerular feedback mechanism involves the juxtaglomerular apparatus (JGA) and a paracrine signaling mechanism utilizing ATP, adenosine, and nitric oxide (NO). This mechanism stimulates either contraction or relaxation of afferent arteriolar smooth muscle cells. Recall that the DCT (Distal Convoluted Tubule) is in intimate contact with the afferent and efferent arterioles of the glomerulus. Specialized macula densa cells in this segment of the tubule respond to changes in the fluid flow rate and Na+ concentration.
- When blood pressure increases for a short duration, more blood flows through the glomerulus and therefore more filtrate is produced.
- This results in a decrease in proximal tubule reabsorption
- This increases the concentration of NaCl in the distal tubule which is detected by the Macula Densa
- The Macula Densa releases local factors resulting in the vasoconstriction of the afferent arteriole
- If blood pressure decreases the opposite occurs
- Vasoconstriction of the afferent arteriole causes a decrease in pressure in the glomerulus and a decrease in GFR, therefore keeping it constant
The following video provides an explanation of the mechanisms of the myogenic response and tubuloglomerular feedback. Start this video at around 2:30 to learn about auto-regulation (the beginning is a review of kidney anatomy).
Renin
Recall our discussions in class about changing the delivery of NaCl to the macula densa. If there is an increase in GFR causing increased release of NaCl to the macula densa in the distal tubule…
- There will be a decrease in the release of renin from the afferent and efferent arterioles
- This will decrease the release of local AII (angiotensin II) which will cause vasodilation of the efferent arterioles greater than the afferent arterioles
- This will decrease GFR, thus keeping it regulated
Tips From Past Students
Renin is an important hormone that functions to regulate the kidneys. It is introduced a little early in this book so do not panic if this is new to you. You can revisit this section after our discussions in class about the hormonal regulation of the kidney and the mechanisms of locally regulating GFR!
Table 1: Summary of the impacts of the constriction of afferent and efferent arterioles on glomerular filtration.
| Arterioles | Resistance (R) | Blood Flow (Q) | Filtration Rate |
|---|---|---|---|
| Constriction of afferent
arteriole (PA) |
Increase | Decrease | Decrease |
| Constriction of efferent
arteriole (PE) |
Increase | Decrease | Increase |
The following video is a valuable resource, as it provides an explanation of how altering the diameter of the afferent and efferent arterioles to/from the glomerulus impacts flow. Skip to 0:46 min and use this to summarize/connect what you have learned.
This image shows the relationship between afferent and efferent arteriolar resistance and how this affects blood flow (RBF), pressure in the glomerulus (PG) and filtration rate (GFR). It will be very helpful to keep these relationships in mind throughout the rest of the kidney unit to help you study and solve problems related to the kidney.

Testing Your Knowledge
Thinking Beyond:
Consider what would happen to filtration in the kidney if an individual had kidney stones that became lodged in the ureter, causing obstruction of the ureter (this would block the flow of urine causing fluid build-up within the nephrons). How would this affect hydrostatic pressure in Bowman’s capsule and GFR?Hint: will increased fluid in the Bowman’s capsule increase or decrease hydrostatic pressure? How does an increase or decrease of the hydrostatic pressure of the Bowman’s capsule affect GFR?
For more information read about urethral obstruction to help with this problem.
Key Takeaways
Consider the following concepts to help guide your studies:
- How a change in pressure will alter the fluid flux.
- The effects of renin on the kidney.
- The difference between autoregulation, myogenic response and tubuloglomerular feedback.
- How each variable in the GFR equation affects GFR when changed.
Sub-chapter Quiz
The questions below can be used to assess your knowledge within this chapter. There are five multiple-choice questions that you should attempt without referring to your notes. The questions will provide you with responses to your answers to guide your studying but should not be used as your only resource.
Media Attributions
- Fluid Flux © Brittany Emary is licensed under a Public Domain license
- Private: Net Filtration Pressue © OpenStax is licensed under a CC BY (Attribution) license
- GFR_Arrows © Brittany Emary is licensed under a CC0 (Creative Commons Zero) license
- Private: Fluid Movement Through Capillaries © Wikimedia Commons is licensed under a CC BY (Attribution) license
- Private: Paracrine Mechanisms Controlling Glomerular Filtration Rate © BC Campus adapted by Brooke Evans is licensed under a CC BY (Attribution) license
- GFR © Brittany Emary is licensed under a Public Domain license
- Myogenic_Response © Brittany Emary is licensed under a Public Domain license
- Arteriole Resistance © Brittany Emary is licensed under a CC0 (Creative Commons Zero) license
- CC BY: Attribution Licensed Content. Edited content. Provided by Lumen Learning. Located at https://courses.lumenlearning.com/cuny-kbcc-ap2/chapter/physiology-of-urine-formation/ ↵
- CC BY: Attribution Licensed Content. Edited content. Provided by Lumen Learning. Located at https://courses.lumenlearning.com/cuny-kbcc-ap2/chapter/physiology-of-urine-formation/ ↵
- CC BY: Attribution Licensed Content. Edited content. Provided by Lumen Learning. Located at https://courses.lumenlearning.com/cuny-kbcc-ap2/chapter/physiology-of-urine-formation/. ↵
- CC BY: Attribution Licensed Content. Edited content. Provided by Lumen Learning. Located at https://courses.lumenlearning.com/cuny-kbcc-ap2/chapter/physiology-of-urine-formation/. ↵
- CC BY: Attribution Licensed Content. Edited content. Provided by Lumen Learning. Located at https://courses.lumenlearning.com/cuny-kbcc-ap2/chapter/physiology-of-urine-formation/. ↵
- CC BY-SA: Attribution-ShareAlike Liscenced content. Edited Content. Provided by Wikimedia Commons. Located at https://commons.wikimedia.org/wiki/File:2108_Capillary_Exchange.jpg ↵
- CC BY: Attribution Licensed Content. Edited content. Provided by Lumen Learning. Located at https://courses.lumenlearning.com/cuny-kbcc-ap2/chapter/physiology-of-urine-formation/. ↵
- CC BY: Attribution Licensed content. Edited Content. Provided by BCcampus. Located at https://opentextbc.ca/anatomyandphysiology/chapter/25-7-regulation-of-renal-blood-flow/ ↵
- CC BY: Attribution Licensed content. Edited Content. Provided by BCcampus. Located at https://opentextbc.ca/anatomyandphysiology/chapter/25-7-regulation-of-renal-blood-flow/ ↵
- CC BY-NC-ND: Attribution-NonCommercial-No Derivatives Licensed Content. Provided by OER Commons. Located at https://www.oercommons.org/courses/glomerular-filtration-rate/view. ↵
- CC BY-NC-ND: Attribution-NonCommercial-No Derivatives Licensed Content. Provided by OER Commons. Located at https://www.oercommons.org/courses/glomerular-filtration-rate/view. ↵
- CC BY-NC-ND: Attribution-NonCommercial-No Derivatives Licensed Content. Provided by OER Commons. Located at https://www.oercommons.org/courses/glomerular-filtration-rate/view. ↵
- CC BY-SA: Attribution-ShareAlike Liscenced content. Edited Content. Provided by Lumen Learning. Located at https://courses.lumenlearning.com/boundless-ap/chapter/body-fluids/ ↵
In the kidney, filtration indicates the movement of water and substrates from the plasma into the renal tubule.
In terms of kidney physiology, reabsorption is when the kidney removes water and solutes from the nephron and returns them to circulation.
In terms of the kidney, whatever fluid remains in the tube is released from the body to the external environment.
The pressure that blood exerts on the walls of vasculature at the level of capillary. This force drives the movement of fluid from the blood into the interstitium.
The osmotic force generated by the presence of proteins in the blood that draws fluid from the interstitium into the vasculature.
The component of the nephron that is responsible for the filtration of blood.
A network of nerves that activate the sympathetic nervous system.
Nerves that innervate the sympathetic nerves of the autonomic nervous system.
Relaxation of smooth muscle cells and the widening of blood vessels. This will allow for more blood flow through the vasculature.
Contraction of smooth muscle cells and the tightening of blood vessels. This will allow for less blood flow through the vasculature.
An enzyme produced by the granular cells of the afferent arteriole at the JGA. It enzymatically converts angiotensinogen to angiotensin I.
A potent vasoconstrictor that plays an immediate role in the regulation of blood pressure.
A hormone that is released from the adrenal cortex in response to angiotensin II or in direct response to an increased plasma K+ concentration. It promotes Na+ reabsorption by the nephron, promoting the retention of water.
Densely packed specialized cells on the wall of the distal convoluted tubule (DCT), found at the point where the thick ascending limb meets the DCT.

