Pulmonary Blood Flow
Pulmonary circulation is defined as the blood flow that is directed towards and through the lungs. It is not the flow to several other tissues and organs around the body known as systemic circulation. The blood flow through the pulmonary circulation is as follows; the right ventricle, pulmonary artery, alveoli, pulmonary vein, left atria. This is essential for gas exchange at the lung. It is important to note that bronchial circulation is not the same as pulmonary circulation, as it is still part of the systemic circulation. It is also functionally different as it supplies the pulmonary structures with the exception of the alveoli and therefore is not crucial for gas exchange.
Learning Outcomes
In this section you will learn…
- What factors cause a change in smooth muscle function to regulate vascular radius.
- How transmural pressure affects alveolar vessels and extra alveolar vessels.
- The different ways in which gravity has an impact on blood flow across the lung.
- How and why laying down versus standing upright affects blood flow across the lung.
Pulmonary Circulation
The vascular radius, as you may recall, is a crucial player in pulmonary circulation. With this, you may also remember that blood vessel radius is vital for predicting the resistance of flow through the system, which is demonstrated in the equation below. In this section, we will examine several ways to regulate vascular radius.
[latex]R=\frac{1}{r^4}[/latex]
This learning object is included to review and solidify the concepts of respiration anatomy discussed in the previous chapter using a 3-dimensional model. The video will further introduce blood flow in the pulmonary system, more specifically pulmonary circulation. A visualization of the respiratory pathway can be seen at the timestamp of 0:15 – 0:30. Make a note of the steps taken to prepare the air before entering the lower respiratory tract, like moistening and warming. The gas exchange process is also touched on within this video at the timestamp of 0:45 – 2:59. Appreciate the intricate network of capillaries that encompass the alveoli, as these vessels are essential moving forward in blood gas exchange.
Change in Smooth Muscle Function
Blood vessels contain smooth muscle, which can be acted on by nervous, endocrine, and paracrine systems to constrict or dilate the vessels. Local control is the first way that smooth muscle function can be altered, meaning that the alveolar partial pressure of oxygen (PO2 ) can dictate whether a vessel will dilate or constrict within the lung. This regulatory method’s innervation comes from the autonomic nervous system, which further branches into the sympathetic (SNS) and the parasympathetic nervous systems (PNS). Recall that the SNS signals during ‘fight or flight’ and the PNS signals the body to act for ‘rest and digest’ functions. Before moving forward, think about how the body would want to alter blood vessel radius during each stage and why.
Test Your Knowledge
Real-Life Scenario:
When standing in line for a study snack, you consciously start to notice your relaxed breathing pattern. You begin to wonder what factors affect the size of your vessels before your next big inhale of that sweet coffee aroma. What are the different effects that may occur? Hint: Think about the different systems that can affect the dilation and constriction of smooth muscle.
We will now look at how the neural pathways mentioned above will influence endocrine stimulation. The endocrine system controls smooth muscle function through alpha and beta-adrenergic receptors. During SNS innervation, epinephrine and norepinephrine hormones are released to interact with beta-adrenergic receptors, causing blood vessels to vasoconstrict. On the opposing end, during PNS innervation, acetylcholine is released, causing blood vessels to vasodilate. Now moving from a full-body endocrine situation, it is essential to look at how cells communicate with each other. Paracrine singling is a type of local cell communication produced by a single cell to stimulate change in their close-by neighbouring cells. Regarding the respiratory tract, the trachea houses epithelial cells capable of releasing products into the smooth muscle to regulate radius. The products released are known as epithelial-derived relaxing factors (EpDRF) and lead to smooth muscle vasodilation.
Smooth muscle function is also influenced by the gasses we inspire, transmural pressure, and autonomic reflexes. For example, if oxygen availability decreases and altitude increases, it causes vasodilation to allow more oxygen to enter the system. Simultaneously, an alteration in transmural pressure according to inhalation or exhalation results in a change in smooth muscle radius. Finally, a reflex such as a cough to expel a liquid or solid object from our airways demonstrates vasoconstriction. This is more of a defensive action in the process of protecting the respiratory system from foreign particles. As you can see, there are multiple ways to alter the respiratory system’s smooth muscles to either encourage vasoconstriction or dilation.
Tips From Past Students
This section of the unit is more or less dependent on memorization and understanding. It is advised that you find ways to test yourself on the effects of each input and the status of the blood vessel radius within the lung.
This section of the blood gases unit requires you to actively recall which inputs lead to vasoconstriction and vasodilation, respectively. This quiz is designed to help you classify the type of inputs that will lead to constriction and dilation within the respiratory tract. After reviewing the section, attempt this from memory to determine which inputs may require further review.
Transmural Pressure and the Effect of Vasculature Radius
We have two main types of vessels that can affect vasculature radius. Extra alveolar vessels, including arteries, arterioles, or veins that are not directly associated with the alveoli. These vessels sit in the thoracic cavity and are part of the pulmonary circulation but are not directly associated with the capillaries. In contrast, alveolar vessels are capillaries that are directly associated with the alveoli. These vessels wrap around the alveoli and allow oxygen to pass from the alveoli into the blood. The big difference between these two vessels is their relationship with resistance during inspiration. During inspiration, the resistance in the extra alveolar vessels will be reduced. While in the alveolar vessels, an increase in resistance is experienced.
Test Your Knowledge
Real-Life Scenario:
Your roommates are studying for a physiology exam and they ask you to help them understand a concept because you are a master of physiology. They ask you how the 2 main types of vessels respond in regard to resistance, during inflation of the lungs? Why? What process is occurring during inflation? Give her some concise notes to help them remember. Hint: Refer back to your anatomy and flow equation to help your roommate.
It can be seen that the alveolar-capillary vessel is crossing over and wrapping around the alveoli, as shown in figure 1. The pressure in the alveoli, in this case, becomes the environmental or transmural pressure and is denoted as PA. When we inspire, the alveoli fill with air and expand, causing an increase in alveolar pressure (PA).
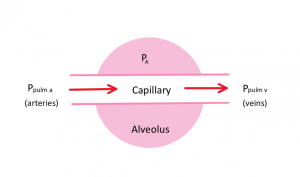
Since the capillary is wrapped around the alveoli, we need to consider three pressures when thinking about blood flow through the capillary, the pressure in the alveoli (PA), the pulmonary artery pressure (PPulmA), and the pressure in the pulmonary vein (PPulmV). To simulate flow through the alveoli-wrapped capillaries, we must be in a situation that allows for the following pressure relationship.
[latex]P_{PulmA} > P_{PulmV} > P_A[/latex]
This video provides an in-depth explanation of the different zones within the lungs and how transmural pressure influences capillary blood flow within the pulmonary circulation. The Starling Resistor Model showcases the impact of flow on various pressure changes within the pulmonary system and is analyzed at the timestamp 4:05 – 6:44. During 9:13- 10:54 the video showcases different pressure gradients within the lungs and how these zones lead to no flow, reduced or intermittent flow, and continuous blood flow.
Let’s practice how the uneven distribution of pressures across the lungs impacts the pulmonary capillary blood flow. Work through these questions to see what topics may need some additional review. Remember, to get flow (Q) we must have a larger pressure on the pulmonary artery side compared to the pulmonary vein side of a capillary; pressure one must be larger than pressure to according to the flow equation.
[latex]Q=\frac{P_1−P_2}{R}[/latex]
Pressure and Blood Flow Across the Lung
There is an inverse relationship between the height of the lung and blood flow, which means that the top region of the lung has the least amount of blood and the bottom of the lung gets the most blood flow. However, this only holds true when an individual is in an upright position, and we will examine why this is later in this chapter section.
Test Your Knowledge
Real-Life Scenario:
How would blood flow differ between different regions of the lung when you are doing a handstand? Why is this different from when you are standing upright? Would the flow be more similar to standing or doing a handstand when you are lying down, or would it be different? Hint: Think about the orientation of the lungs and how they would be affected by gravity.
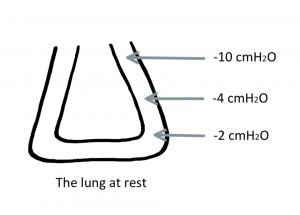
Many structures have an uneven distribution of pressures across their entire surface, and the lung is no different. When we are standing in an upright position, we can think of the lung as having three distinct flow levels due to pressure differences. At the top of our lungs, we have no flow (Q). This is due to the alveoli’s pressure being more significant than the pulmonary artery pressure, shown in figure 2. While in the middle of the lung, we see intermittent or reduced blood flow, and by the time we reach the bottom of the lung, we see a continuous stream of flow through the vasculature.
Key Takeaways
Consider the following concepts to help guide your studies:
- The four key factors that can cause a change in smooth muscle function to regulate vascular radius are neural, endocrine, paracrine, and local control.
- The specific mechanisms at which these sections cause this regulatory function are dependent upon the system that initiated them.
- Transmural pressure in the extra alveolar vessels will be reduced during inspiration due to the alveolar vessels increasing in pressure, thus pushing against the non-associated vessels.
- The inverse height-blood flow relationship within the lungs leads to the formation of three different pressure zones.
- The top region of the lung having the lowest cmH2O concentration in comparison to the bottom region.
- This lower pressure causes the top of the lungs to obtain the least amount of blood flow.
Subchapter Quiz
The questions below have been created to assess your knowledge within this chapter. You will find multiple-choice questions that will provide you with responses to your answers. Be sure to review any remaining sticky spots and critical points after you’ve completed them.
Media Attributions
- Blood Flow Through the Alveolus © Santana Ferreira is licensed under a CC BY (Attribution) license
- Lung Pressures © Santana Ferreira is licensed under a CC BY (Attribution) license
The blood flow that is directed towards and through the lungs.
The delivery of oxygen from the inhaled air in the lungs into the blood and the removal of carbon dioxide from the blood into the exhaled air in the lungs.
Mechanisms through which organs and tissues alter themselves independent of nerves or hormones.

