Sex Hormones
This subchapter covers the overall roles of the male and female reproductive systems. We will explore how the menstrual cycle causes hormonal changes in females and the role of the testes and the process of spermatogenesis in males. The changes that occur during puberty will be discussed as well. You will learn how different hormones come into play in these systems, when and why they are required, and their regulation throughout the system with respect to positive and negative feedback. You will learn about the physiological effects of arousal and how ejaculation occurs to result in fertilization.
Learning Outcomes
In this section you will learn…
- Endocrine and paracrine control of sex hormones in both males and females.
- The changes in the hormonal profile that occur during each phase of the menstrual cycle.
Male Sex Hormones
Testosterone is a steroid hormone produced primarily in the male testes and is responsible for the secondary sexual characteristics in males after puberty. These secondary sex characteristics include a deepening of the voice, the growth of facial, axillary, and pubic hair, and increased sex drive.[1] Testosterone levels fluctuate throughout the lifespan. An increase in testosterone at puberty marks the transition from a non-reproductive to a reproductive state. Throughout adulthood, testosterone levels remain relatively constant until old age, when levels gradually decline. Sex glands and their related hormones need to be tightly regulated to allow for the production, development and maturation of gametes. In the male, gametes are produced in the testes.
The following video is a good overview of the anatomy of the male reproductive system, however, covers some material that your are not expected to know! This can be used as background information and does not need to be a main focus of study.
The Testes
The primary role of the testes are to produce testosterone and provide a suitable environment for the production and maturation of sperm through a process called spermatogenesis. Spermatogenesis takes place in the Seminiferous tubules of the testes and relies on three different cell types: Sertoli cells, Peritubular Cells and Leydig cells.
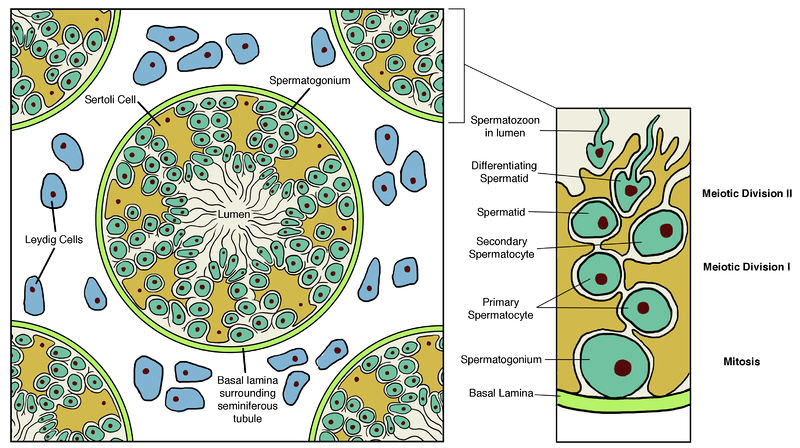
The image below shows the different cell types of the testes and seminiferous tubules. Note the location of Leydig and Sertoli cells, and of maturing sperm.
Cell Types Involved in Spermatogenesis
Seminiferous tubules are made up of a single cell layer comprised of Sertoli cells. Adjacent Sertoli cells provide the space where meiosis occurs and where male gametes (sperm) are produced. Sertoli cells play a crucial role in secreting hormones and factors that promote the development and maturation of sperm cells.
Leydig cells lie adjacent to the seminiferous tubules, and are stimulated to produce testosterone.
Peritubular cells, which lie on the surface of the seminiferous tubules, are smooth muscle cells that can contract. [2] These contractions are responsible for the rhythmic, wave-like nature of sperm production, meaning that all sperm at one stage of maturation will progress to the next stage of maturation at the same time. Note in Figure 1, that the most mature, differentiated, sperm are found closest to the lumen of the seminiferous tubule, and that the immature sperm are found closest to the basal membrane. Contraction of the peritubular cells moves the sperm closer to the lumen as it matures. The lumen of the seminiferous tubule is connected to the epididymis and vas deferens which carries the sperm to ejaculatory ducts for expulsion. Peritubular cells also secrete proteins that act on other nearby cells, in a paracrine manner.
This wave-like, uniform, maturation requires an immense amount of paracrine integration and input from nearby Leydig, Peritubular and Sertoli cells. The rest of this section will focus on explaining how these cells work alongside endocrine mechanisms to achieve this.
Tips From Past Students
Remember peristalsis and how food is propelled through your digestive tract? Sperm mature in the same way. Through the contraction of muscle-like cells, sperm are propelled to the next stage of maturation towards the lumen of seminiferous tubules.
Paracrine Regulation of Male Sex Hormones
LH from the anterior pituitary stimulates Leydig cells to produce testosterone. Testosterone affects nearby tissues in a paracrine manner and distant tissues in an endocrine manner. Locally, testosterone acts on Peritubular cells and Sertoli cells. In Peritubular cells, testosterone stimulates the production of activating proteins. In turn, these activating proteins, together with testosterone, stimulate Sertoli cells to secrete important growth factors and proteins. Sertoli cells will also produce inhibin, activin, proteins, and estradiol, all of which feedback onto Leydig cells. The feedback role of the secretions produced by Sertoli cells is summarized in the table below.
| Hormones | Type of Feedback |
|---|---|
| Activin | negative feedback on Leydig cells |
| Estradiol | negative feedback on Leydig cells |
| Activating proteins | positive feedback on Leydig cells |
| Inhibin | positive feedback on Leydig cells |
In this pathway, positive feedback onto Leydig cells will produce more testosterone, whereas negative feedback will stop testosterone production. Overall, the purpose of paracrine regulation, and multiple levels of control is to control testosterone levels to ensure an optimal environment within the testes for the maturation of sperm.
The purpose of the following diagram is to demonstrate how testosterone production is regulated and the role of each cell type on controlling testosterone production. Note that the blue arrows symbolize updating mechanisms between germ cells and sertoli cells.
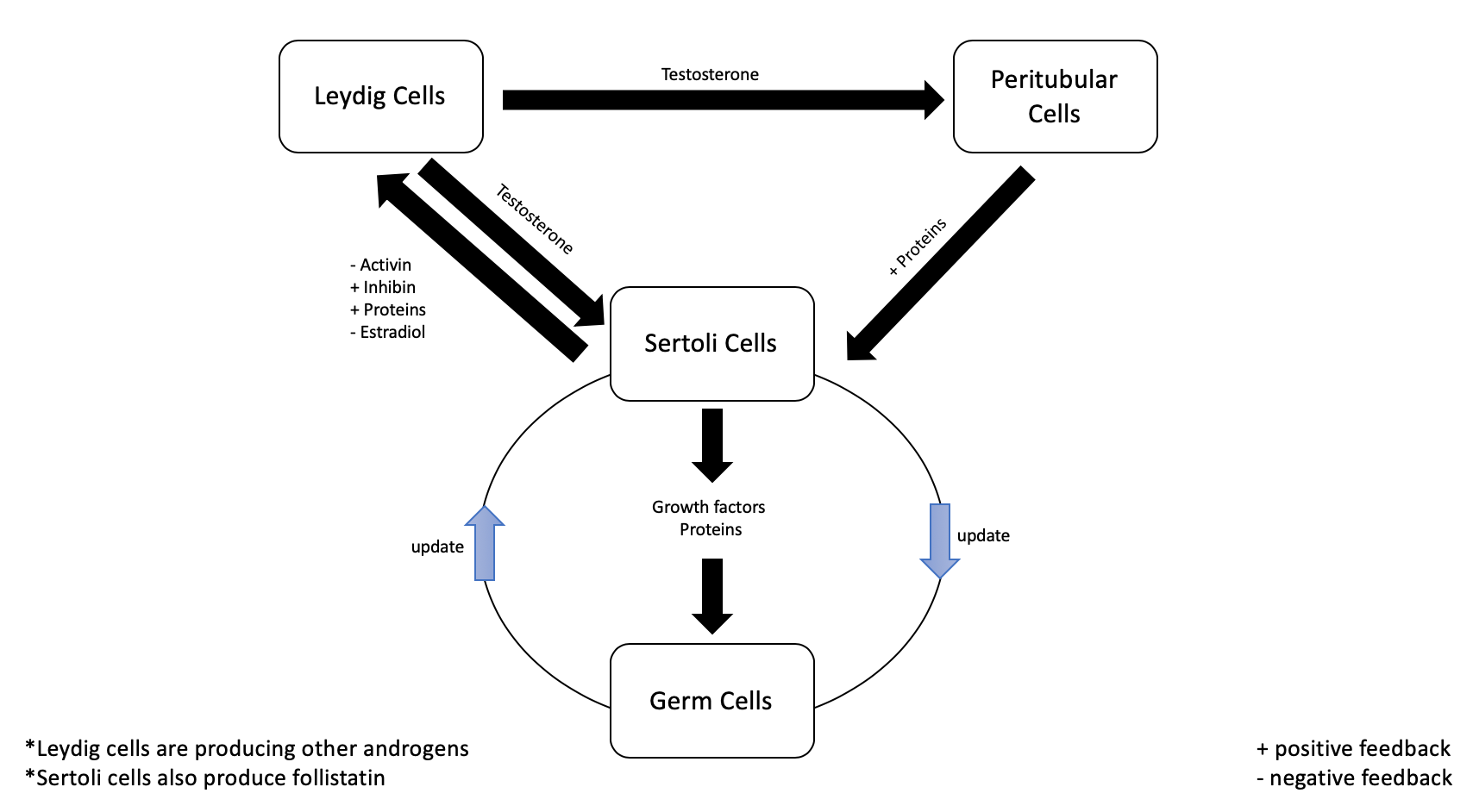
As we discussed previously, sperm will mature in ‘waves’ and are produced between the space of two adjacent Sertoli cells. Consequently, there has to be some type of communication between germ cells and Sertoli cells that allows for the coordinated movement of sperm between compartments. Although this pathway has not been explicitly identified, there must be a mechanism where germ cells provide updates to Sertoli cells on maturation stage.
Tips From Past Students
The role of activin and inhibin switches depending on whether or not we are looking at a paracrine or endocrine control of sex hormones. In paracrine control, activin will inhibit (less testosterone production) and inhibin will activate (more testosterone production). In endocrine control, activin will activate (more testosterone production) and inhibin will inhibit (less testosterone production).
Endocrine Regulation of Male Sex Hormones
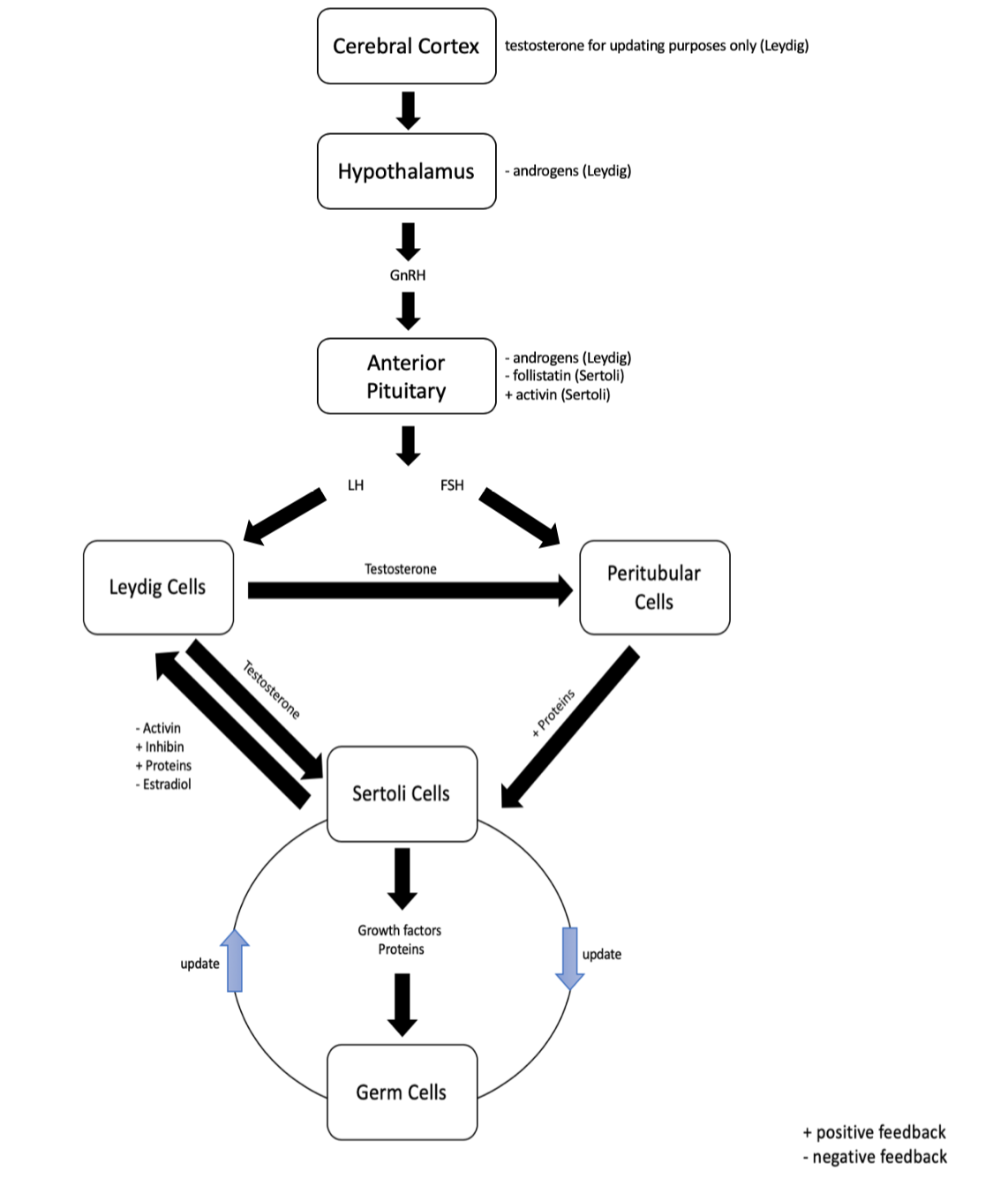
The diagram below contains very important information that should be studied thoroughly. You should be able to describe the process of sperm production and how it is regulated by hormonal control. The green (left) and red (right) colour systems in this diagram will help you contrast the different hormonal inputs that are involved in the maintenance and maturation of spermatozoa.
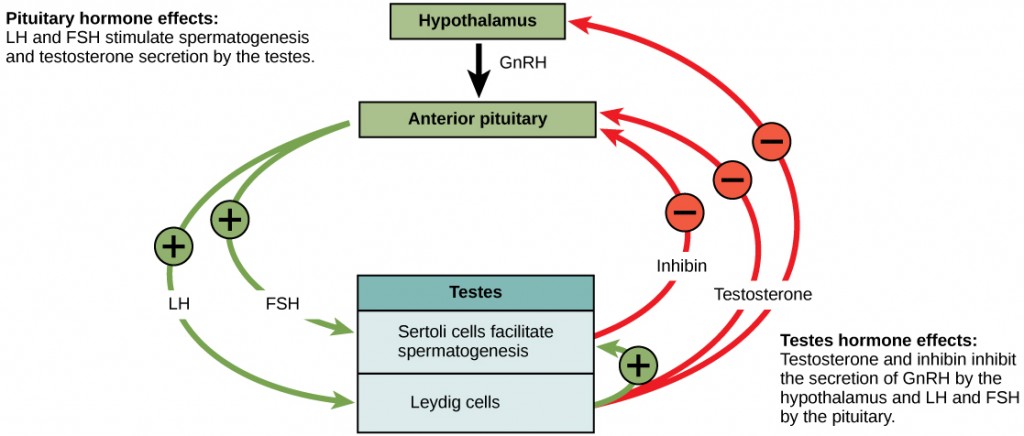
At the onset of puberty in males, the hypothalamus starts secreting Gonadotropin releasing hormone (GnRH) which acts on the pituitary gland to release FSH and LH. FSH acts on Sertoli cells to stimulate the production of inhibin, growth factors, activin and follistatin. LH acts on Leydig cells to stimulate the production of testosterone and androgens. All of these hormones and growth factors work together to provide an optimal environment for the maturation of sperm. This process describes endocrine regulation because these hormones (FSH, LH) are produced centrally and are secreted into the blood, where they eventually arrive at the testicles to elicit a response.
The products of Leydig cells and Sertoli cells are summarized in the table below.
| Hormones | Type of Feedback |
|---|---|
| Testosterone and androgens (Leydig) | negative feedback on the hypothalamus and anterior pituitary |
| Inhibin (Sertoli) | negative feedback on anterior pituitary |
| Activin (Sertoli) | positive feedback on anterior pituitary |
| Follistatin (Sertoli) | negative feedback on anterior pituitary |
As depicted in figure 3, rising levels of testosterone act on the hypothalamus and anterior pituitary to inhibit the release of GnRH, FSH, and LH.[3] Sertoli cells which produce the hormone inhibin and follistatin when sperm count is high and exhibits negative feedback on the anterior pituitary, decreasing the release of FSH and LH into the blood.[4] A decrease in FSH and LH causes a sub-optimal environment for sperm production, and leads to a decline in spermatogenesis.[5] If the sperm count reaches 20 million/ml, the Sertoli cells stop secreting inhibin, and stops negative feedback which initiates spermatogenesis once again.[6] In contrast, the hormone activin initiates positive feedback on the anterior pituitary which stimulates the release of FSH and LH.
Testosterone also acts on the cerebral cortex, however it does not exhibit any type of feedback. Rather, testosterone works on the cerebral cortex to relay information for updating purposes. For example, this updating pathway would communicate current testosterone levels to the brain.
The diagram below depicts how male sex hormones are regulated by endocrine control. Note the effect of hormones on target tissues and the negative feedback mechanisms that control hormone release.
Physiological Effects of Arousal
In order for fertilization to occur, two important factors are required: a female and an erection.
Penile Erection
When physical or physiological stimulation occurs, the parasympathetic nervous system (PNS) is activated. With the PNS activated, the secretion of the neurotransmitter acetylcholine (ACh) is released and acts on the endothelial cells (EC) in the microvasculature of the penis. This stimulates the release of nitric oxide (NO) onto the vascular smooth muscle cells of the penis. Nitric oxide activates guanylate cyclase, which converts guanosine triphosphate to cyclic guanosine monophosphate (cGMP). An increase in cGMP causes a decrease in calcium levels, leading to vasodilation of smooth muscle cells and engorgement. The process is summarized in a step by step process below:
- Activation of PNS
- ACh release
- ACh acts on EC of penis
- Increase NO release from EC
- NO acts on vascular smooth muscle
- Increase guanylate cyclase activity
- Increase cGMP
- Decrease Ca2+ levels
- Relaxation vascular smooth muscle
- Vasodilation
- Engorgement
To stop an erection, cGMP phosphodiesterase will act to decrease total cGMP. This is achieved by converting cGMP to 5’GMP. This reduces vasodilation, which stops an erection.
The following diagram demonstrates what happens when an erection stops. This simple learning object is here to provide a visual representation of the concept. You should know how to describe this pathway.
Ever wonder how viagra works? Viagra is a drug that males with erectile dysfunction can take to maintain an erection. This drug works by inhibiting cGMP phosphodiesterase, and stops the conversion of cGMP to 5’GMP, a process that was encountered in the vision section. This drug is taken orally, and is distributed systemically and will inhibit the enzyme anywhere it is present in the body, causing systemic side effects. Because viagra inhibits cGMP phosphodiesterase, one of the most common side effects of viagra is vision problems. Notably, the most dangerous side-effects of viagra occurs more commonly in men who have heart problems and are taking nitrates. Nitrates work to vasodilate coronary arteries and treat chest pain. Because viagra also works as a vasodilator, men who take both nitrates and viagra may experience a drastic decrease in blood pressure which can be very dangerous. [7]
Test Your Knowledge
Thinking Beyond:
Using what we have learned about male Viagra, describe another strategy you could use to maintain an erection. Hint: Think about the steps involved in developing a penile erection, and discuss if there’s some way you could alter these steps to maintain the erection.
Penile Ejaculation
There are two phases involved with penile ejaculation: emission and expulsion. In order for ejaculation to occur, the male must have mature spermatozoa in seminiferous tubules. Once the spermatozoa are mature within the seminiferous tubule and the physiological/physical stimulation is present, the spermatozoa can then move to the epididymus. From the epididymis, the sperm then travel to the vas deferens, then the ejaculating duct and to the penis. This is the onset of orgasm and once this has started, the man likely will continue to ejaculate and orgasm fully, with or without further stimulation.[8] If sexual stimulation stops before orgasm, the physical effects of the stimulation, including the vasocongestion, will subside in a short time.[9]
The learning object below is above the course level. The important takeaway from this diagram is that the anterior pituitary and hypothalamus are very sensitive to negative feedback before puberty. After puberty, sensitivity decreases and the anterior pituitary is stimulated to produce LH and FSH. Please do not memorize all of the secondary sex characteristics, but note the difference in hormonal regulation between males and females.
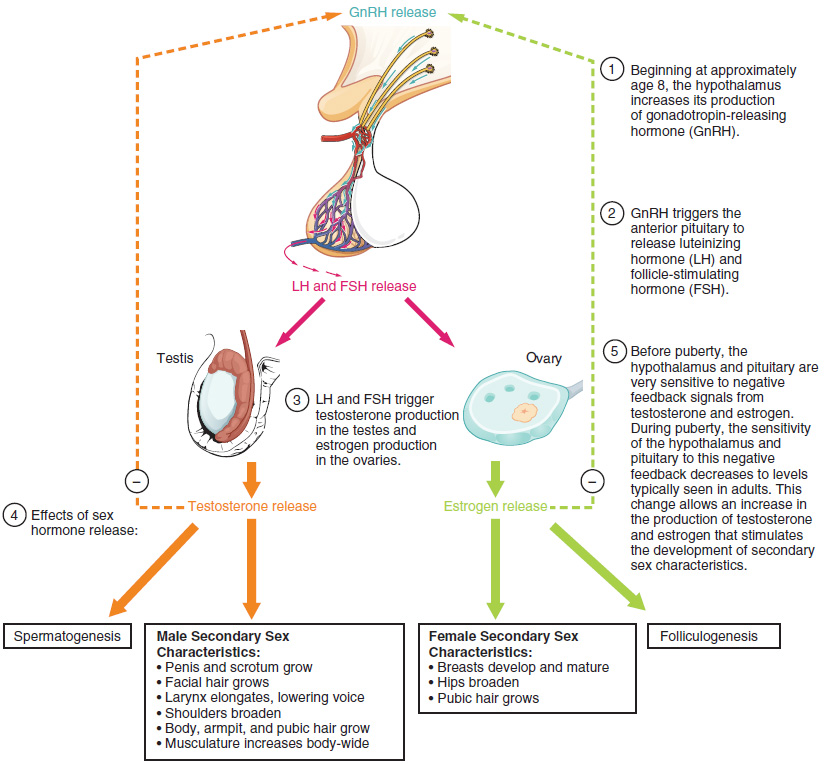
Tips From Previous Students
Before puberty, estrogen and testosterone feedback on the hypothalamus and prevent GnRH release. This is negative feedback! Make sure you are keeping these bigger concepts and themes in mind as you move through this course.
Test Your Knowledge
Clinical Application:
We can apply our knowledge of male sex hormones to the new strategies being developed for “male birth control”. These include either stopping sperm maturation or inhibiting ejaculation of mature spermatocytes. What are some other specific strategies you could use to develop this sort of birth control. Hint: Think about the hormones involved in spermatogenesis and how you might modify this process. You could also consider the process of ejaculation and think about ways you could prevent this event from leading to pregnancy in a female.
Female Sex Hormones
The ovarian cycle governs the preparation of endocrine tissues and release of eggs, while the menstrual cycle governs the preparation and maintenance of the uterine lining.[10] These cycles occur concurrently and are coordinated over a 22–32 day cycle, with an average length of 28 days.[11]
The two primary sex organs in the female reproductive system are the ovaries and the uterus. During the menstrual cycle, various changes occur to these organs to allow for conception. During the menstrual cycle, the ovaries function to develop and mature the oocyte while the uterus develops an environment in which the fertilized egg will be housed.
The two primary sex hormones produced in females are estrogen and progesterone. These two hormones work alongside luteinizing hormone (LH) and follicle-stimulating hormone (FSH) to regulate the female menstrual cycle.
Phases of the Menstrual Cycle
The menstrual cycle is made up by three distinct phases: Follicular, Ovulatory and Luteal Phase.
Follicular Phase – Before release of egg
Ovulatory Phase – Release of egg
Luteal Phase – After egg release
The following diagram will help you connect the changes in the uterus and ovaries in accordance with hormone level changes during the different stages of the menstrual cycle.
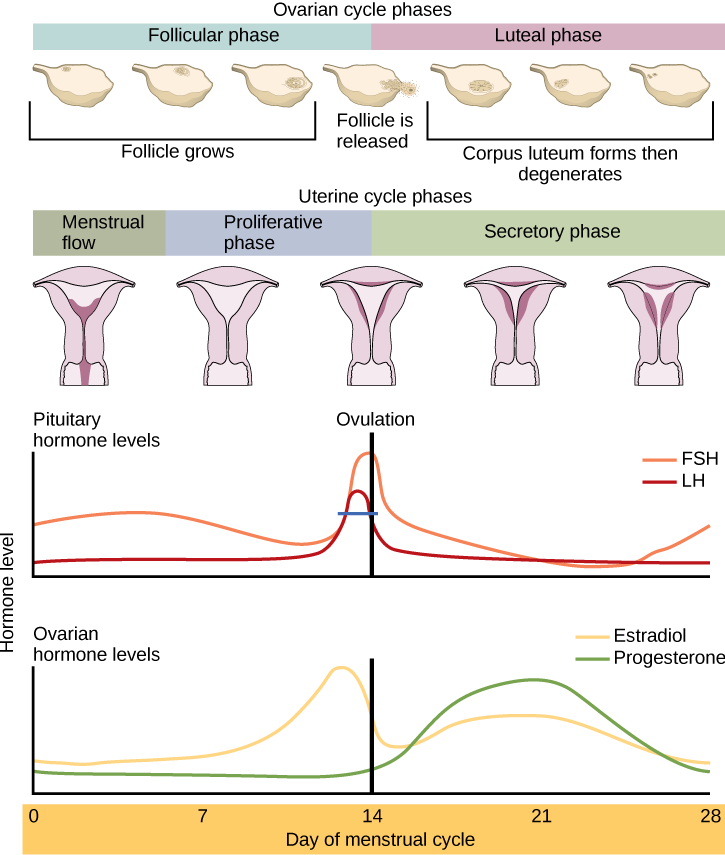
Tips From Past Students
Take note how the spike in LH triggers the release of the egg from the follicle in the ovaries, as well as how the development of the corpus luteum produces an increase in both progesterone and estradiol levels.
Follicular Phase
The first half of the ovarian cycle is the follicular phase shown in Figure 7.[12] Slowly rising levels of FSH and LH cause the growth of follicles on the surface of the ovary, preparing the egg for ovulation. As the follicles grow, they begin releasing estrogens and a low level of progesterone.[13] Progesterone maintains the endometrium to help ensure pregnancy. The trip through the fallopian tube takes about seven days.[14] If pregnancy implantation does not occur, the lining is sloughed off. After about five days, estrogen levels rise and the menstrual cycle enters the proliferative phase.[15] The endometrium begins to regrow, replacing the blood vessels and glands that deteriorated during the end of the last cycle.[16]
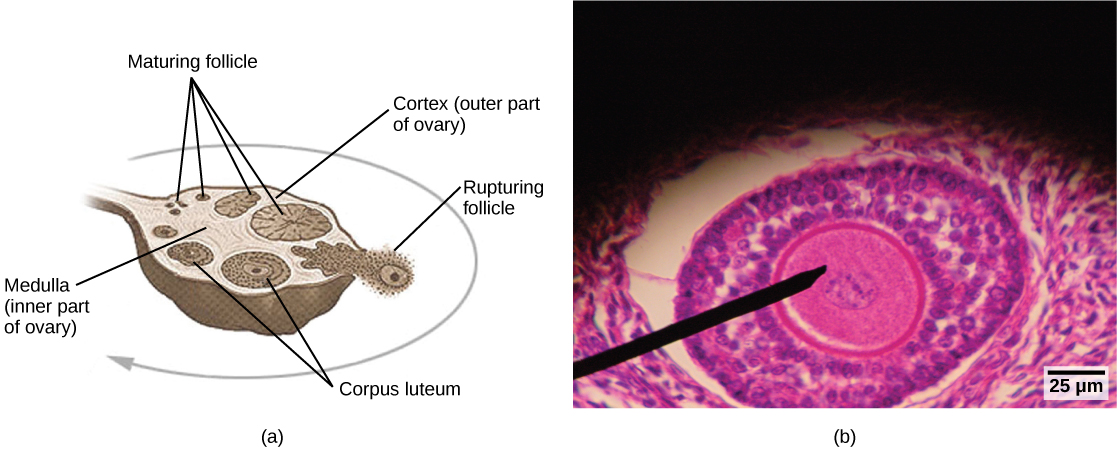
Ovulatory Phase
Just prior to the middle of the cycle (approximately day 14), the high level of estrogen causes FSH and especially LH to rise rapidly, then fall. The spike in LH causes ovulation: the most mature follicle, like that shown in Figure 8, ruptures and releases its egg.[17] The follicles that did not rupture degenerate and their eggs are lost. The level of estrogen decreases when the extra follicles degenerate.[18]
Luteal Phase
Following ovulation, the ovarian cycle enters its luteal phase, illustrated in Figure 7 and the menstrual cycle enters its secretory phase, both of which run from about day 15 to 28.[19] The luteal and secretory phases refer to changes in the ruptured follicle. The cells in the follicle undergo physical changes and produce a structure called a corpus luteum. The corpus luteum produces estrogen and progesterone.[20] The progesterone facilitates the regrowth of the uterine lining and inhibits the release of further FSH and LH. The uterus is being prepared to accept a fertilized egg, should it occur during this cycle. The inhibition of FSH and LH prevents any further eggs and follicles from developing, while the progesterone is elevated.[21] The level of estrogen produced by the corpus luteum increases to a steady level for the next few days.[22]
The image below shows how mature follicles rupture, release an egg and leave behind a corpus luteum. Think about the changes in the sex hormone profile that occur with each step!
If no fertilized egg is implanted into the uterus, the corpus luteum degenerates and the levels of estrogen and progesterone decrease.[23] The endometrium begins to degenerate as the progesterone levels drop, initiating the next menstrual cycle. The decrease in progesterone also allows the hypothalamus to send GnRH to the anterior pituitary, releasing FSH and LH and starting the cycles again.[24] Figure 9 visually compares the ovarian and uterine cycles as well as the commensurate hormone levels.[25]
The learning object below demonstrates the female sex hormone levels during the menstrual and ovulation cycles. Think about the feedback mechanisms and how GnRH and FSH/LH is regulated at each stage in the cycle. How does the hormone profile change at each step? You are not expected to know all of the details in the figure.
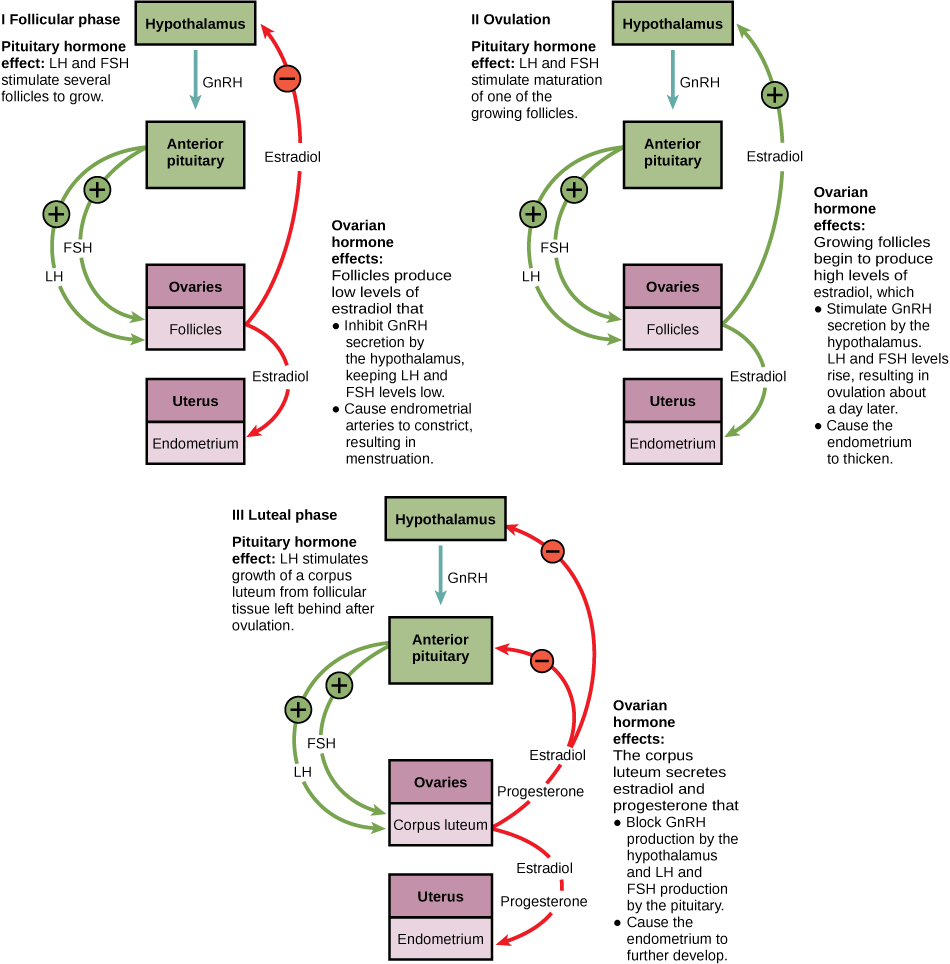
Tips From Past Students
This is a great diagram depicting the negative and positive feedback regulation that happens in the menstrual and ovarian cycles. What are other examples where you have encountered negative and positive feedback regulation?
Are you interested in learning more about female sex hormone disorders? Polycystic ovary syndrome (PCOS)is a disorder of the female reproductive system which causes high levels of testosterone. In PCOS many follicles will grow in the ovaries (“polycystic”), where the eggs remain immature. Because there is no ovulation, it alters the female sex hormone profile to cause higher levels of testosterone than normal. Testosterone disrupts the menstrual cycle, therefore people with PCOS will often have fewer periods. Overall PCOS can cause fertility problems, diabetes and the development of male secondary sex characteristics like facial hair. Treatment of PCOS is often individualized, and focusses on addressing specific symptoms. For example, to reduce hair growth or regulate the menstrual cycle, a doctor might prescribe birth control pills.[26]
Endometriosisis a disorder characterized by the growth of endometrial tissue, outside of the endometrium in the uterus. The hormonal changes that occur during the menstrual cycle also affect the tissue growing outside of the uterus. Over time, this leads to the formation of scar tissue, fertility problems and pain in the pelvic region. Treatment may involve pain management and hormone therapy; however, severe forms of disease may require surgery to remove scar tissue from the pelvic area.[27]
Test Your Knowledge
Clinical Application:
Let’s see how our knowledge of female sex hormones can be applied to the following applications.
Intrauterine Devices (or IUDs) are a form of female birth control that in some cases use progesterone. How would high levels of progesterone throughout the menstrual cycle prevent fertilization of an ovum?
Adenomyosis is a condition in which the endometrium grows inside the muscle lining of the uterus. It can result in infertility. Describe how infertility might result. Hint: Think about the role of the endometrium throughout the menstrual cycle, and what it does when an ovum is fertilized.
Key Takeaways
Consider the following concepts to help guide your studies:
- Understand how hormones control primary and secondary male characteristics.
- How feedback loops control the regulation of sex hormones for spermatogenesis and the menstrual cycle.
- The physiological process of male arousal.
- Know what occurs at each stage of the menstrual cycle and how an egg is released.
- Understand how sex hormones are regulated by paracrine and endocrine control.
Subchapter Quiz
Below you will find a short quiz to test your knowledge from this subchapter. This will be a good indicator of how well you understand the content or can be used to review for the final exam.
Media Attributions
- Cross Section of Testis © Laura Guerin is licensed under a CC BY-NC (Attribution NonCommercial) license
- Paracrine regulation of male sex hormones © Jennifer St. Amant is licensed under a CC BY (Attribution) license
- Hormonal Regulation of Sperm Production © Molnar, C. and Gair, J. is licensed under a CC0 (Creative Commons Zero) license
- Endocrine Regulation of Male Sex Hormones © Jennifer St. Amant is licensed under a CC BY (Attribution) license
- cGMP phosphodiesterase
- Female and Male Hormone Secretion © Wikimedia Commons is licensed under a CC BY-SA (Attribution ShareAlike) license
- Cyclic Secretion: Ovarian Cycle © OpenStax CNX is licensed under a CC BY (Attribution) license
- Menstrual cycle and ovulation is licensed under a CC0 (Creative Commons Zero) license
- The Negative Feedback Loop of the Ovarian Cycle © Lumen Learning is licensed under a CC0 (Creative Commons Zero) license
- Lumen (n.d.) Hormonal Control of Human Reproduction. Boundless Biology. ↵
- Punwani, V. (n.d.). Spermatogenesis. Khan Academy. ↵
- Lumen (n.d.) Hormonal Control of Human Reproduction. Boundless Biology. ↵
- Lumen (n.d.) Hormonal Control of Human Reproduction. Boundless Biology. ↵
- Lumen (n.d.) Hormonal Control of Human Reproduction. Boundless Biology. ↵
- Lumen (n.d.) Hormonal Control of Human Reproduction. Boundless Biology. ↵
- Davis, C.P. (2016). Erectile Dysfunction (ED) Causes and Treatment. MedicineNet. ↵
- Lumen (n.d.) Physiology of the Male Reproductive System. Boundless Openstax. ↵
- Lumen (n.d.) Physiology of the Male Reproductive System. Boundless Openstax. ↵
- Lumen (n.d.). The Ovarian Cycle, the Menstrual Cycle, and Menopause. Biology for Majors II. ↵
- Lumen (n.d.). The Ovarian Cycle, the Menstrual Cycle, and Menopause. Biology for Majors II. ↵
- Lumen (n.d.). The Ovarian Cycle, the Menstrual Cycle, and Menopause. Biology for Majors II. ↵
- Lumen (n.d.). The Ovarian Cycle, the Menstrual Cycle, and Menopause. Biology for Majors II. ↵
- Lumen (n.d.). The Ovarian Cycle, the Menstrual Cycle, and Menopause. Biology for Majors II. ↵
- Lumen (n.d.). The Ovarian Cycle, the Menstrual Cycle, and Menopause. Biology for Majors II. ↵
- Lumen (n.d.). The Ovarian Cycle, the Menstrual Cycle, and Menopause. Biology for Majors II. ↵
- Lumen (n.d.). The Ovarian Cycle, the Menstrual Cycle, and Menopause. Biology for Majors II. ↵
- Lumen (n.d.). The Ovarian Cycle, the Menstrual Cycle, and Menopause. Biology for Majors II. ↵
- Lumen (n.d.). The Ovarian Cycle, the Menstrual Cycle, and Menopause. Biology for Majors II. ↵
- Lumen (n.d.). The Ovarian Cycle, the Menstrual Cycle, and Menopause. Biology for Majors II. ↵
- Lumen (n.d.). The Ovarian Cycle, the Menstrual Cycle, and Menopause. Biology for Majors II. ↵
- Lumen (n.d.). The Ovarian Cycle, the Menstrual Cycle, and Menopause. Biology for Majors II. ↵
- Lumen (n.d.). The Ovarian Cycle, the Menstrual Cycle, and Menopause. Biology for Majors II. ↵
- Lumen (n.d.). The Ovarian Cycle, the Menstrual Cycle, and Menopause. Biology for Majors II. ↵
- Lumen (n.d.). The Ovarian Cycle, the Menstrual Cycle, and Menopause. Biology for Majors II. ↵
- Watson, S. (2019). Polycystic Ovary Syndrome (PCOS): Symptoms, Causes, and Treatment. healthline. ↵
- Mohamed, A.W. (2019). Endometriosis. healthline. ↵
Period of time at which a person is first capable of sexual reproduction.
The male gonads in animals.
Male gametes.
The process of sperm production within the seminiferous tubules in the testes.
The site of male gamete production (spermatogenesis).
Cells that secrete a number of growth factors and activating proteins to ensure an optimal environment for spermatogenesis. This process is stimulated by FSH.
Cells that contract and propel sperm to the next location where it will continue to mature.
Adjacent to the seminiferous tubules, these interstitial cells produce testosterone in the presence of LH. Numerous factors secreted by other cells act on leydig cells to regulate testosterone production.
The process in which a single cell divides twice to produce four daughter cells. Each cell has one copy of each chromosome. In males, this process usually produces four viable gametes. In females, only one gamete is typically produced.
The reproductive cells of an organism.
A tube behind the testis that carries sperm to the vas deferens.
The duct in the testes that carries semen from the epididymis to the ejaculatory duct.
The forcible ejection of semen from the mammalian urethra, a reflex in response to sexual stimulation.
In this cycle, an ovarian follicle matures and ruptures, releasing an egg, eventually forming a corpus luteum.
Female gametes.
A process that thickens the lining of the uterus and prepares it for implantation of an egg (pregnancy). If there is no pregnancy (egg), there will be menses, the sloughing of the uterine lining.
A hormone produced by gonadotropic cells of the anterior pituitary gland. It triggers ovulation and development of the corpus luteum in females and stimulates production of testosterone of leydig cells in males.
Stimulates the growth and recruitment of immature ovarian follicles in females. In males, it is critical for spermatogenesis as it stimulates primary spermatocytes to form secondary spermatocytes.
The inner lining of the uterus that grows to become thick, and vascular in preparation for pregnancy.
After the release of the egg from the follicle, a corpus luteum is formed. The role of the corpus luteum varies depending on whether or not pregnancy occurred.

