Muscle Contraction
Something as simplistic as walking to class, or eating a banana is a much more involved process than the superficial and visual aspect, which has been becoming ever more clear throughout this chapter. This subchapter will expand on your knowledge from the previous subchapters to focus on how nerves are able to communicate with muscle fibers and create muscular contractions. Neuro-muscular communication is one of the many highly integrated components involved in the aforementioned examples. This subchapter will also introduce the characteristics and organization of muscle tissues to understand how structural differences in a muscle allow for different contractions to be formed.
Learning Outcomes
In this section you will learn…
- Appreciate the different types of muscle tissue.
- Describe the organization of sarcomeres, myofibrils, and muscle fibers.
- Understand the structure and components of a sarcomere.
- Explain the process of skeletal muscle contraction.
- Differentiate between calcium ion sources in skeletal muscle and cardiac muscle.
- Recognize the structural differences between smooth and striated muscle and the relation to contraction.
Types of Muscle Tissue
The following image provides a visual representation of the three different types of muscle tissue found in humans and an example of each. Types of muscle tissue are not a huge focus of the course but are important background information to keep in mind as you move through the unit. This image is at course level. However, do not focus on differentiating between the muscle types visually.
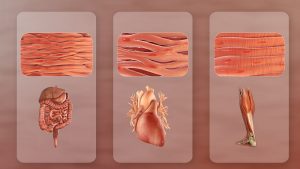
As can be seen in the above photo, there are three types of muscle tissue: smooth muscle, cardiac muscle, and skeletal muscle. Cardiac and skeletal muscles are both subtypes of striated muscle. Striated muscle is named due to its appearance under a microscope, but is beyond the scope of this course. The appearance and organization of the muscle fibers vary among the different muscle types, and they are found in different locations in the body. Cardiac muscle is found solely in the heart and is responsible for the involuntary contractions that pump blood around your body. Smooth muscle is also under involuntary control and is found in a wide array of organs, including the intestines, urinary bladder, and blood vessels. Skeletal muscle is the only muscle type under voluntary control and is attached to your bones across joints to produce movement during contraction.
Tips from Past Students
Of the three muscle types, skeletal muscle is the primary focus of HK*2810. Many concepts are identical between the three muscle types, but there are some key differences as well. You will learn more about smooth muscle and cardiac muscle during HK*3810.
The Organization of a Striated Muscle Fiber
The following image provides a visual for the structure of a muscle fiber and shows the location of sarcomeres within myofibrils. The different levels of organization within muscles may seem confusing, but this image helps because it focuses on the structure of the cell itself, and the sarcomere, its functional unit. This image is at course level. However, don’t worry about being able to label the muscle fiber. Rather, focus on the organization of myofibrils within muscle fibers and sarcomeres within myofibrils.
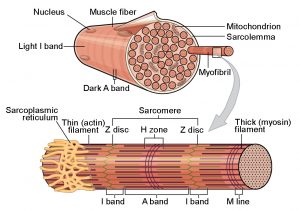
Muscle fibers are the cells that make up muscle tissue. Muscle fibers look a little different than the typical cell diagrams that you see during high school biology classes. Muscle fibers are elongated and cylindrical. The cell membrane of a muscle fiber is called the sarcolemma, and the cytoplasm is called the sarcoplasm. Muscle fibers also have a structure called the sarcoplasmic reticulum, which is similar to the endoplasmic reticulum and stores calcium ions (Ca2+). Hundreds to thousands of myofibrils are also found within one muscle fiber. The myofibrils are elongated threads that run parallel to each other and contain the sarcomeres. The sarcomeres are the contractile units of the muscle fibers and are arranged consecutively, separated by Z lines (Z discs).
Did you know the prefixes “myo-” and “sarco-” originate from the Greek words? “Mu”, means “muscle”, and “sark”, means “flesh”. When you hear these prefixes, you can be confident that the word is related to muscles (ex. “myofibrils”, “myofilaments”, “sarcomeres”, “sarcolemma”).
Test Your Knowledge
Real-Life Scenario:
Pretend you are working out at the gym and tracking your strength progress. After consistently working out for 4 months, you have noticed your muscles have increased in size and you have gotten stronger. What adaptations are the muscles making to increase in size and strength? Hint: What functional component of the muscle could increase its population to increase force production?
The Structure of a Sarcomere
The following image shows the organization of a sarcomere and zooms in on portions of the thick and thin filaments. As you look through this image, try and connect the various labeled components to their role in muscle contraction. As well, pay attention to the relationship between troponin, tropomyosin, and actin.
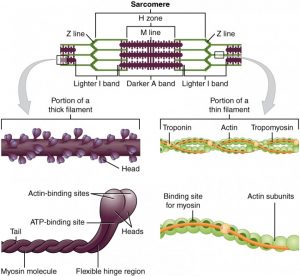
Sarcomeres are composed of thin (actin) filaments and thick (myosin) filaments. Actin is anchored to z-lines. Myosin is freely mobile and its heads interact with actin for contraction. The myosin heads cannot bind anywhere on actin but rather, must interact with the binding sites on actin. However, while the muscle is relaxed, the binding sites for myosin are covered by the troponin-tropomyosin complex. The steps taken to create a muscle contraction are discussed later in this subchapter.
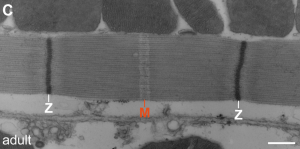
Are you interested in learning more about the sarcomere? The following image shows an electron micrograph of a sarcomere. One sarcomere runs between the two Z-lines (the white Zs). The lighter areas directly beside the Zs represent the regions where only thin filaments (actin) are found. The region labeled “M” is the area where only thick filaments (myosin) are found. The region between the exclusively actin and myosin regions are where both types of filaments overlap. This electron micrograph helps to visualize where the actin and myosin get their names of “thin” and “thick” filaments, respectively. The individual myosin filaments can be seen because of their thickness, but individual actin filaments cannot be seen because they are so thin.
Tips from Past Students
One way to remember the organization of sarcomeres within a myofibril is to think about the z-lines. The z-lines are the part of the sarcomere that look like the letter “z”. The letter “z” indicates the end of the alphabet and the z-line indicates the ends of the sarcomeres.
Skeletal Muscle Contraction
The following diagram outlines the process of muscle contraction, beginning with the arrival of an action potential at a neuromuscular junction, and ending with a shortening of the muscle. This image is useful because it provides a big picture explanation of the mechanisms of muscle contraction, without focusing too much time on the smaller details. This diagram is below course level as it is only a summary, and you will be required to know more of the biochemical details.

The process of muscle contraction (excitation-contraction coupling) is as follows:
- An action potential arrives at a neuromuscular junction.
- As a result of the action potential reaching the end of the axon and depolarizing it, acetylcholine (ACh) is released from the neuron and binds to receptors on the muscle fiber, opening sodium ion channels.
- The influx of sodium ions causes an action potential along the sarcolemma.
- The action potential travels down t-tubules along the sarcolemma.
- This membrane depolarization causes the opening of calcium channels on the sarcoplasmic reticulum, leading to increased intracellular calcium concentrations.
- Calcium binds to troponin, which moves tropomyosin from the myosin-binding sites on actin.
- Actin and myosin can now interact.
- Myosin binds ATP and hydrolyzes it to ADP and Pi. This causes a conformational change in the myosin heads.
- The myosin heads pull on actin, causing the sarcomeres to shorten and resulting in muscle contraction.
Test Your Knowledge
Thinking Beyond:
Using what you know about the steps to contract a muscle. Write out the steps for relaxation of a muscle. Hint: What needs to stop occurring/ stop being released in order for the contraction to stop?
The video below provides a review of the process of skeletal muscle contraction. This is a helpful video because it allows you to see the actin and myosin interaction, and therefore muscle contraction, in action.
0:00-1:20 Muscle physiology
1:20 Sliding filament theory
3:35 Calcium release
This video is slightly below course level, as it does not include as many details as you will learn during lecture. However, watching all the steps come together in action can provide a strong framework to understand muscle contraction.
Remember that all the myosin heads of a sarcomere act independently. In order for movement to occur, all the myosin heads, on all the sarcomeres, within all the myofibrils, within a muscle fiber, must contract at the same time, and the muscle will shorten. Muscles have tendons that terminate at joints. When the muscle contracts, the tendon pulls on the joint, changing the angle of the two bones connected by the joint, and producing movement.
Ever wonder how Rigor Mortis works? After death, the body is no longer producing ATP, therefore, muscle contraction cannot be undone. This causes permanent muscle contraction.
Skeletal Muscle Calcium Sources
The following image provides an overview of sources of calcium in skeletal muscle cells. This image is at course level. However, don’t worry about knowing the “terminal cisternae”. It simply refers to the enlarged area of the sarcoplasmic reticulum.
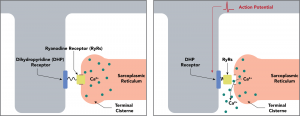
Calcium is the second messenger involved in muscle contraction. In order for actin and myosin interaction to occur, calcium must be present inside the muscle fiber. In skeletal muscle, the calcium ions are stored in the sarcoplasmic reticulum. When the sarcolemma is depolarized, the local current travels along the t-tubules and causes the voltage-dependent dihydropyridine receptor to change shape, yank on the ryanodine receptor and open a calcium channel on the surface of the sarcoplasmic reticulum. Intracellular calcium levels increase. Increased intracellular calcium increases the force of contraction and decreased intracellular calcium decreases the force of contraction.
Tips from Past Students
Once intracellular calcium levels increase, the process of muscle contraction is identical in both types of striated muscle (skeletal and cardiac muscle). However, prior to this step, there are small differences between the two types. We focus on skeletal muscle during HK*2810, and you will learn more about cardiac muscle during HK*3810.
Cardiac Muscle Calcium Sources
The diagram below shows the sources of calcium for cardiac muscle contraction. As well, the diagram provides a strong overview of the mechanisms by which calcium is recycled during cardiac muscle relaxation.
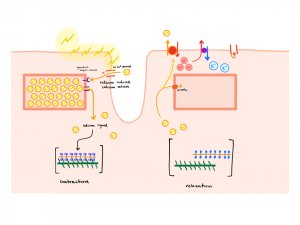
Cardiac muscle fibers receive calcium from two sources: the sarcoplasmic reticulum and intracellularly. The calcium channels on the sarcoplasmic reticulum are ligand-gated. The ligand that must bind to open these channels is calcium. This is referred to as calcium-induced calcium release (CICR) because calcium both binds the channel and passes through the channel. The calcium that binds the channel is called “trigger calcium” and comes from extracellular sources. However, there is no difference between the extracellular calcium and the calcium from the sarcoplasmic reticulum. They are identical. In order to decrease intracellular calcium levels for muscle relaxation to occur, there are three mechanisms that the cell utilizes:
-
- A calcium ATPase on the sarcoplasmic reticulum.
- A calcium ATPase on the cell membrane.
- A calcium/sodium exchanger on the cell membrane. This exchanger makes use of the sodium concentration gradient set up by the sodium/potassium ATPase also on the cell membrane. While it moves sodium with its concentration gradient, it is able to move calcium against its concentration gradient.
Test Your Knowledge
Thinking Beyond:
What might happen to the heart if the calcium ATPase pumps on the sarcoplasmic reticulum in cardiac myocytes are defective? What effect might this have on heart rate? Heart contractility Contractility is the force or strength of contraction. Hint: Will the cardiac myocytes be able to contract and relax normally?
Smooth Muscle Contraction
The image below shows the interaction between dense bodies, thin filaments, and thick filaments in smooth muscle tissue. It provides a nice visual for how all these components work together to cause muscle contraction. You learn how one set of dense bodies, thin filaments, and thick filaments cause muscle contraction, but it can be tricky to see the big picture and think about how multiple sets work together, which is why this picture can be so useful.
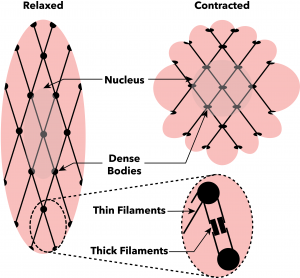
The structure of smooth muscle is different than that of striated muscle. Smooth muscle fibers do not have sarcomeres. However, they do have thin and thick filaments. Where the thin filaments are anchored to the Z-line in striated muscle, they are instead anchored to dense bodies in smooth muscle. Many thin filaments can be anchored to one dense body. Similar to striated muscle, myosin pulls on actin during contraction. This causes the dense bodies to move closer together and causes shortening of the muscle fiber.
Tips from Past Students
Think about concentric (shortening) muscle contraction like this… Imagine you’re standing between two bookshelves (bookshelves= z-discs), one on either side of you, and your goal is to bring them together. There are ropes tied to the bookshelves that you can pull to slide the shelves along. (your arms= myosin, ropes= actin). You repetitively pull the ropes towards you, regrasp it and then pull again. This is the actin and myosin interacting to shorten the muscle. Once the bookshelves are right beside you, there is no more myosin that your actin/arms can interact with. That is when no more tension can be produced.
The diagram below provides a nice visual of the process of smooth muscle contraction. It is a helpful resource as it shows the process in a different way by using images, rather than just words. This image is slightly below course level as it does not go into as much detail as your notes, however, it is a nice overview to begin with.
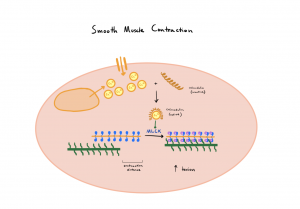
The steps of smooth muscle contraction are listed below (as shown in figure 10):
- Cytoplasmic levels of calcium (Ca2+) increase in smooth muscle cells from both extracellular and intracellular sources.
- Ca2+ binds the inactive form of calmodulin, activating it.
- The calmodulin-Ca2+ complex then binds myosin light chain kinase (MLCK).
- The calmodulin-Ca2+-MLCK complex activates myosin via the addition of an ATP molecule.
- Myosin cleaves the ATP to form ADP and Pi. This is the form of myosin that binds actin, causing muscle contraction.
Test Your Knowledge
Clinical Application:
Suppose you are designing a drug that relieves hypertension. If hypertension is high blood pressure caused by increased contraction of smooth muscle in the blood vessels, propose a mechanism for this drug. Hint: What receptor would it bind to? What cellular changes would it induce in the cells it binds to?
Key Takeaways
Consider the following concepts to help guide your studies:
- Smooth, Cardiac, and Skeletal are the three types of muscle tissues within the human body
- Muscle fibres are functionally organized, consisting of a series of myofibrils, each formed by several sarcomeres separated by Z-lines.
- Within the sarcomere, actin is anchored to Z-lines and myosin is free to move. Contraction causes a power stroke to occur between actin and myosin, pulling Z-lines towards each other and shortening the muscle.
- For a contraction to occur, an AP from the neuromuscular junction travels down the sarcolemma causing a membrane depolarization that opens calcium channels on the sarcoplasmic reticulum. This increases intracellular calcium binding to troponin, removing tropomyosin from myosin-binding sites on actin, enabling actin and myosin to interact using ATP to perform a power stroke.
- Within skeletal muscle, calcium ions are stored in the sarcoplasmic reticulum and are released following depolarization down the sarcolemma and t-tubules. Cardiac muscle, however, uses extracellular calcium in addition to stores within the sarcoplasmic reticulum. As well, rather than being voltage gated as in skeletal muscle, cardiac muscles sarcoplasmic reticulum’s are ligand gated.
Subchapter Quiz
The questions below can be used to assess your knowledge within this chapter. There are five multiple-choice questions that you should attempt without referring to your notes. The questions will provide you with responses to your answers to guide your studying but should not be used as your only resource.
Media Attributions
- Types Of Muscle © Scientific Animations Inc. is licensed under a CC BY-SA (Attribution ShareAlike) license
- Private: Muscle Types © Ghaid Asfour is licensed under a All Rights Reserved license
- Muscle Fiber © Rice University is licensed under a CC BY (Attribution) license
- Thick and Thin Filaments © Rice University is licensed under a CC BY (Attribution) license
- Electron microscopy of developing and adult flight muscle myofibrils © Loison O, Weitkunat M, Kaya-Çopur A, Nascimento Alves C, Matzat T, Spletter ML
- Contraction © Oregon State University is licensed under a CC BY-SA (Attribution ShareAlike) license
- Coupling of the Muscle Action Potential to Calcium Release from the Sarcoplasmic Reticulum © Daniel Walsh and Alan Sved is licensed under a CC BY-SA (Attribution ShareAlike) license
- Calcium_and_cardiac_muscle_contraction © David Nascari and Alan Sved is licensed under a CC BY-SA (Attribution ShareAlike) license
- Smooth Muscle Cell Contraction © Daniel Walsh and Alan Sved is licensed under a CC BY-SA (Attribution ShareAlike) license
- Calcium and Smooth Muscle Cell Contraction © David Nascari and Alan SVed is licensed under a CC BY-SA (Attribution ShareAlike) license
One of the three types of muscle tissue found in the human body. Smooth muscle is under involuntary control and is found in a variety of internal organs, including the intestines, bladder, and blood vessels.
One of the three types of muscle tissue found in the human body. Cardiac muscle is under involuntary control and is found solely in the heart.
One of the three types of muscle tissue found in the human body. Skeletal muscle is under voluntary control and is attached to your joints to produce movement during contraction.
A muscle cell.
The cell membrane of a striated muscle cell.
The cytoplasm of a striated muscle cell.
A structure, similar to the endoplasmic reticulum, that is found in striated muscle fibers. Its main function is to store calcium ions.
The contractile unit of a muscle fiber, composed of sliding protein filaments of actin and myosin.
One of the two protein filaments that make up a sarcomere; thin filament.
One of the two protein filaments that make up a sarcomere; thick filament.
A protein complex that covers the binding sites for myosin on actin.
The process of turning an action potential into a muscle contraction.
A change in membrane potential that passes along a neuron or muscle fiber to transmit an impulse.
A chemical synapse formed between a motor neuron and a muscle fiber.
Extensions of the cell membrane that go into the centre of striated muscle fibers at the Z-lines.
The release of calcium from the sarcoplasmic reticulum, which is triggered by the binding of calcium to the ligand-gated channels on the sarcoplasmic reticulum.
A structure found in smooth muscle fibers that thin filaments anchor to. Dense bodies are analogous to z-lines in striated muscle.