Tubular Reabsorption
The fluid that flows through the glomerulus and Bowman’s capsule after filtration is called the filtrate. Recall that filtrate contains water and other important solutes. You might think that the kidney acts a giant sieve for the body, ridding it of unwanted junk. And you would be partially correct, but remember the kidney also acts to keep substances that are wanted by the body! Tubular [pb_glossary id=”1524″]reabsorption[/pb_glossary] mechanisms in the nephrons move solutes and water out of the filtrate back into the bloodstream, to ensure that these are not lost in the urine. In addition to the reabsorption of important substances, the nephron is also able to secrete unwanted substances from the bloodstream into the filtrate, a process rightfully named secretion. Together, these two processes complete the transformation of the filtrate into the urine. This section will discuss how important substances move between the membranes of the kidney and the results of these processes. Before we get into that, we will first review the mechanisms through which ions and other substances can cross cellular membranes.
Learning Outcomes
In this section you will learn…
- Describe the movement of solutes between membranes in the kidney.
- Describe reabsorption and secretion in the proximal convoluted tubule, distal convoluted tubule, and the loop of Henle.
- Describe and apply your knowledge of the countercurrent multiplier system.
- Apply your knowledge of the collecting ducts and the recovery of water.
Mechanisms of Recovery
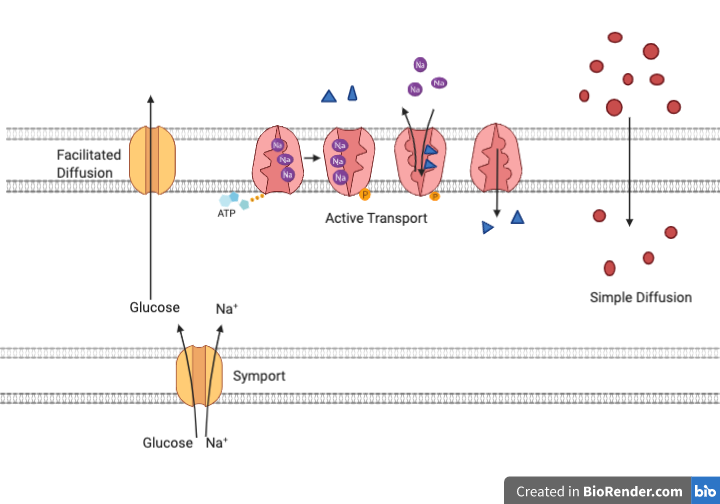
Reabsorption and secretion include mechanisms of active transport, diffusion, facilitated diffusion, secondary active transport, and osmosis to move substances across membranes.
- Active transport uses energy (ATP), to move a substance across a membrane from an area of low concentration to an area of high concentration against the concentration gradient. An example would be the active transport of sodium out of the cell and potassium into a cell by the Na+/K+ antiport, moving the ions in opposite directions.
- Simple diffusion moves a substance from an area of higher to an area of lower concentration down its concentration gradient. It requires no energy and only needs the substance to be soluble.
- Facilitated diffusion is similar to simple diffusion in that it moves a substance down its concentration gradient. The difference is that it requires specific membrane receptors or channel proteins for movement. An example would be the movement of glucose, and in certain situations, sodium. In some cases of mediated transport, two different substances share the same channel protein port; these mechanisms are described by the terms symport and antiport.
- When active transport powers the transport of a secondary substance in this way, it is called secondary active transport. An example would be glucose reabsorption in the kidneys. Na+/K+ ATPases on the basal membrane of a tubular cell constantly pump sodium out of the cell, maintaining a strong electrochemical gradient for sodium to move into the cell from the tubular lumen. On the luminal surface, a sodium/glucose symport protein assists both sodium and glucose movement into the cell. The cotransporter moves glucose into the cell against its concentration gradient as sodium moves down the electrochemical gradient created by the basal membranes. The glucose molecule then diffuses across the basal membrane by facilitated diffusion into the interstitial space and from there into it moves into the peritubular capillaries.
Most calcium, sodium, glucose, and amino acids must be reabsorbed by the nephron to maintain homeostatic plasma concentrations. Other substances such as urea, potassium, ammonia, creatinine, and some drugs are secreted as waste products. Acid-base balance is maintained through the secretion or reabsorption of hydrogen and bicarbonate. See figure 1 below for a visual representation of the mechanisms of transport discussed.
Tips From Past Students
It might be helpful to go through the sections of your notes about reabsorption along with the several parts of the nephron, then revisit this section to help clarify the mechanisms used for reabsorption. Focus on understanding it to help with your knowledge of fluid flux in the kidney.
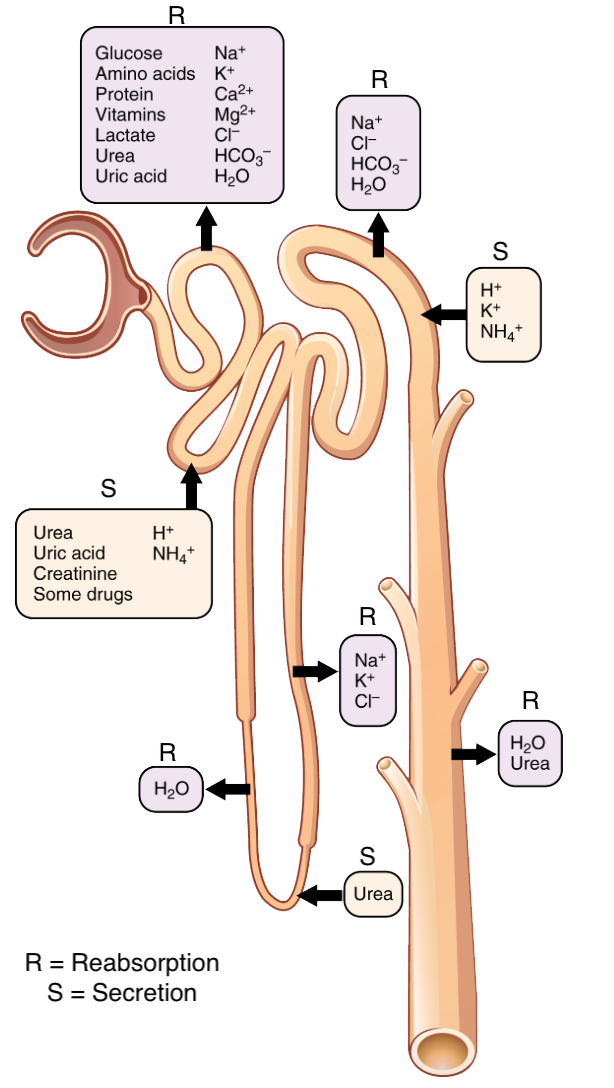
It is extremely important to know what substances are being secreted and reabsorbed by the nephron and where this is occurring, Figure 2 below outlines these locations. It is also important to understand why certain substances are secreted or reabsorbed at certain locations throughout the nephron, and what factors may increase or decrease reabsorption or secretion. For example, the secretion of the antidiuretic hormone will increase water reabsorption. Remember that any substance leaving the nephron (reabsorbed) is entering the bloodstream via the peritubular capillaries or vasa recta and will stay in the body. Any substance brought back into the nephron (secretion) will be excreted from the body.
| Substance | PCT | Loop of Henle | DCT | Collecting Duct |
| Glucose | ~100% reabsorbed; Secondary active transport with Na+ | |||
| Proteins and amino acids | ~100% reabsorbed; symport with Na+ | |||
| Vitamins | Reabsorbed | |||
| Lactate | Reabsorbed | |||
| Creatinine | Secreted | |||
| Urea | 50% reabsorbed by diffusion; also secreted | Secretion, diffusion in descending limb | Reabsorption in medullary collecting ducts; diffusion | |
| Sodium (Na+) | 65% actively reabsorbed | 25% reabsorbed in thick ascending limb; active transport | 5% reabsorbed; active | 5% reabsorbed, stimulated by aldosterone (ALDO); active |
| Chloride (Cl–) | Reabsorbed, symport with Na+, diffusion | Reabsorbed in thin and thick ascending limb; diffusion in ascending limb | Reabsorbed; diffusion | Reabsorbed; symport |
| Water | 67% reabsorbed osmotically with solutes | 15% reabsorbed in descending limb; osmosis | 8% reabsorbed if Antidiuretic hormone (ADH); osmosis | Variable amounts reabsorbed, controlled by ADH, osmosis |
| Bicarbonate (HCO3–) | 80-90% symport reabsorption with Na+ | Reabsorbed, symport with Na+ and antiport with Cl–; in ascending limb
|
Reabsorbed; diffusion | Reabsorbed antiport with Cl–
|
| H+ | Secreted; diffusion
|
Secreted; active
|
Secreted; active
|
|
| Ammonium (NH4+) | Secreted; diffusion
|
Secreted; diffusion
|
Secreted; diffusion
|
|
| Some drugs | Secreted
|
Secreted; active
|
Secreted; active
|
|
| Potassium (K+) | 65% reabsorbed; diffusion | 20% reabsorbed in thick ascending limb, symport | Secreted; active
|
Secretion controlled by aldosterone; active
|
| Calcium (Ca2+) | Reabsorbed; diffusion
|
Reabsorbed in thick ascending limb; diffusion
|
Reabsorbed if parathyroid hormone (PTH) present; active
|
|
| Magnesium (Mg) | Reabsorbed; diffusion
|
Reabsorbed in thick ascending limb; diffusion
|
Reabsorbed
|
|
| Phosphate (PO43-) | 85% reabsorbed, inhibited by parathyroid hormone, diffusion
|
Reabsorbed; diffusion
|
Tips From Past Students
Do not focus on memorizing each ion and its permeability, instead try to focus on the key aspects that would influence glomerular filtration rate and renal blood flow. Understand the general trends of each area of the kidney and whether it is permeable to these key ions/substances.
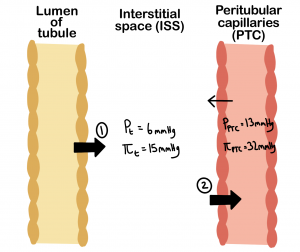
Reabsorption is a two-step process. It begins with the passive or active transport of water and solutes from the fluid in the lumen of the tubule, through the tubule wall, into the interstitial space (ISS). Then there is the passive or active transport of water and solutes from the ISS, through the capillary walls, into the bloodstream. In the kidney, filtration and reabsorption occur across two different capillary beds, the glomerulus and the peritubular capillaries (PTC), respectively. Similar to filtration, reabsorption in the kidney is influenced by hydrostatic and osmotic pressures. The relationship between hydrostatic pressures and osmotic pressures of the tissues, PTC, and Bowman’s capsule is described by the fluid flux equation where Jfluid is fluid flux, CFC is a constant, PPTC is the hydrostatic pressure of the PTC (13mmHg), Pt is the hydrostatic pressure of the tissue (6mmHg), πPTC is the osmotic pressure of the PTC (32mmHg), and πt is the osmotic pressure of the Bowman’s capsule (15mmHg).
[latex]Jfluid = CFC*((PPTC - P_t) - (πPTC - π_t))[/latex]
As you can see from the variables above, there is a very high osmotic pressure in the PTC. This is due to the blood in the PTC being very concentrated as a result of filtering so much fluid out of the blood at the glomerulus. This creates a much larger drive to move fluid osmotically instead of hydrostatically. Remember that water moves to dilute a concentrated area, so water will be drawn to move into the blood since it is very concentrated. In other words, since the change in osmotic pressure (πPTC – πt) is greater than the change in hydrostatic pressure (PPTC – Pt),the net movement of fluid will be from the ISS into the PTC. The diagram below in figure 3 shows the two-step process of reabsorption. First, water and solutes from the lumen of the tubule in the nephron are moved by transporters into the ISS. Second, the osmotic forces drive the movement of solutes and water from the ISS into the PTC.
Reabsorption and Secretion in the Proximal Convoluted Tubule
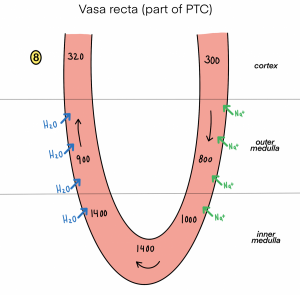
The proximal convoluted tubule (PCT) is the first point at which the forming urine is modified. Here, some substances are reabsorbed, and some are secreted. Water and substances that are reabsorbed are returned to the circulation via the peritubular and vasa recta capillaries. It is important to understand the difference between the glomerulus, peritubular, and vasa recta capillaries. The glomerulus has high pressure and can sustain this by dilating the afferent arteriole while constricting the efferent arteriole to drive substrate movement. In contrast, movement in the peritubular capillaries and the vasa recta is influenced primarily by osmolarity and concentration gradients. Sodium is actively pumped out of the PCT to drive the movement of water into the capillaries.
The majority, about 70%, of reabsorption of substances from the filtrate occurs at the PCT. The kidney is built in terms of cell asymmetry. This means that there are different transporters on each side of the cells to move things in one direction. The movement of important substances from the filtrate in the lumen of the tubule into the ISS occurs through:
- Symporters or antiporters (for glucose, amino acids, phosphate)
- Diffusion of ions (for Na+, Cl–, K+, Ca+)
- Osmosis and aquaporins (for water)
- Endocytosis (for proteins)
Once in the ISS, these substances can be moved into the lumen of the PCT through the osmotic drive discussed above. This two-step process completes reabsorption. It is important to know what substances are secreted and reabsorbed in the PCT. In addition, it may be helpful to learn what channels and transporters are present in the PCT. In figure 4 below, you can visualize the reabsorption and secretion of substances via various channels in the PCT.
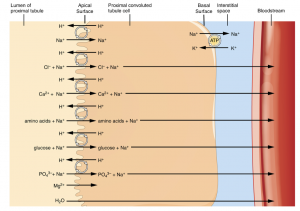
More substances move across the membranes of the PCT than any other portion of the nephron. In fact, about 67% of the water, sodium, and potassium entering the nephron is reabsorbed in the PCT. Cells have two surfaces: the apical and basal. The apical surface faces the lumen or the inside of the PCT. While the basal surface of the cell faces the connective tissue to which the cell attaches, the basement membrane. Pumps and channels vary between the apical and basilar surfaces. A few of the substances that are transported via symport mechanism on the apical membrane include chloride, calcium, amino acids, glucose, and phosphate, which can be seen above in figure 4. Sodium is exchanged with potassium through active transport on the basal membrane.
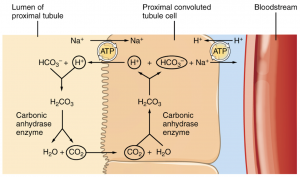
The recovery of bicarbonate is vital for acid-base balance. Carbonic anhydrase (CA) catalyzes this mechanism as shown in figure 5. In the kidney, most of the CA is located within the cell, but a small amount is bound to the brush border of the membrane on the apical surface of the cell. In the lumen of the PCT, bicarbonate combines with hydrogen ions to form carbonic acid (H2CO3). This is catalyzed into carbon dioxide and water, which diffuses across the apical membrane into the cell. Water can move osmotically across the lipid bilayer membrane due to the presence of aquaporin channels. Inside the cell, the reverse reaction occurs to produce bicarbonate ions (HCO3–). These are co-transported with sodium across the basal membrane to the interstitial space (ISS). Simultaneously, a Na+/H+ antiporter excretes hydrogen into the lumen, while it recovers sodium.
HCO3– + H+ ↔ H2CO3 ↔ CO2 + H2O
The recovery of solutes from the lumen of the PCT to the ISS creates an osmotic gradient that promotes the recovery of water. Changing the number of aquaporin proteins on the collecting ducts also helps regulate the osmolarity of the blood.
There is also the secretion of substances at the proximal tubule that are to be eliminated in the urine, such as anions, cations, or bile salts. Secretion is the movement from the peritubular capillaries into the ISS then into the lumen of the tubule through these same transporters mentioned above.
Testing Your Knowledge
Clinical Application:
Diabetes is a common risk factor for kidney disease. In a healthy individual, all of the glucose that was filtered into the nephron is reabsorbed back into the blood at the proximal tubule. However, individuals who are diabetic have high blood glucose levels resulting in excess glucose filtered into the tubule of the nephron. What is one way that you could tell someone is diabetic from testing their urine? Hint: What would be different in their urine from that of a healthy individual?
Reabsorption in the Loop of Henle
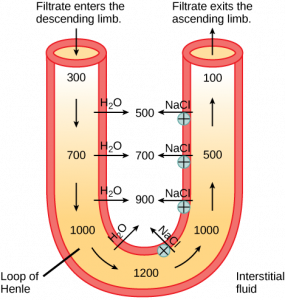
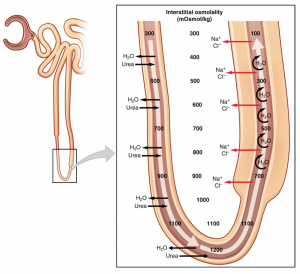
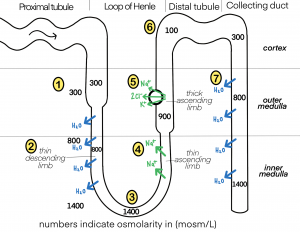
The loop of Henle consists of a thin descending limb, as well as a thick and thin ascending limb. The loop of Henle is specialized to enable the recovery of sodium and water that has been filtered by the glomerulus. Roughly 40% of filtered sodium is reabsorbed in the loop of Henle, primarily in the thick ascending limb. Urine is formed as the filtrate moves through the loop of Henle, creating a cortico-medullar osmotic gradient. This gradient is maintained by the different permeabilities of the different sections of the loop of Henle, the active reabsorption of sodium in the thick ascending limb, and the U-shape of the loop.
As the urine is formed, the osmolarity will change from isosmotic between the lumen of the loop of Henle and the interstitial space to hypertonic. This is a result of osmosis occurring in the descending limb and active transport occurring in the ascending limb. It is also worth noting that the loop of Henle also plays a small role in the reabsorption of filtered bicarbonate. Research has shown that under physiologic conditions, the majority of the bicarbonate reabsorption occurs in the proximal tubule with the loop of Henle playing a modest role. However, bicarbonate concentration increases at the tip of the loop of Henle, as an indirect result of water reabsorption along the descending limb. Therefore, bicarbonate is reabsorbed in the loop of Henle via the transcellular pathway.
Did you know that the ability of kangaroos and rats to produce hyper-concentrated urine is due to their long loop of Henle (proportional to their size)? This is an adaptation for life in the desert so that these animals can maintain their blood volume. [2] The following video describes the reabsorption and secretion of sodium in the loop of Henle and how this affects urine concentration. [3]
Reabsorption in the Descending Limb
The descending limb of the loop of Henle penetrates the medulla and it is comprised of simple squamous epithelial cells. When filtrate enters the descending limb of the loop of Henle it is [pb_glossary id=”8464″]isotonic[/pb_glossary] with the plasma and the interstitial space. The thin descending limb of the loop of Henle does not reabsorb any sodium, and water reabsorption occurs passively via aquaporins, allowing for the unrestricted movement of water. This increases the osmolarity from 300mOsmol/kg to ~1200mOsmol/kg. This increased osmolarity results in about 15% of the water entering the nephron to be reabsorbed.
Reabsorption in the Ascending Limb
Thin Ascending Limb
The thin ascending limb of the loop of Henle is impermeable to water and permeable to sodium. Sodium moves across the epithelium as a result of the differences in osmolarity between the tubule and the interstitial space.
Thick Ascending Limb
The thick ascending limb is lined with simple cuboidal epithelium without a brush border. The thick ascending limb is completely impermeable to water due to the absence of aquaporin proteins; however, sodium and chloride are actively reabsorbed by a co-transport system. Because water is retained as this section is impermeable to water and sodium chloride is removed, the filtrate becomes hypoosmotic as it reaches the distal convoluted tubule. In contrast, the interstitial space (ISS) becomes increasingly hyperosmotic. Active reabsorption of sodium in the thick ascending limb serves two main functions. It allows for the dilution of the luminal fluid as well as the movement of sodium and chloride in the ISS. This contributes to the generation of a strong osmotic gradient in the outer medulla
Na+/K+ ATPases in the basal membrane create an electrochemical gradient. This allows the reabsorption of chloride by Na+/Cl- symporters in the apical membrane. As sodium is actively pumped from the basal side of the cell into the interstitial space, chloride follows sodium from the lumen into the ISS through leaky tight junctions. These leaky tight junctions are found between the cells of the ascending loop, where they allow for the movement of certain solutes. Most of the potassium that enters via symporters returns to the lumen through these leaky channels in the apical membrane. The potassium exits the loop of Henle because the ISS is now a negatively charged environment that attracts cations from the lumen into the ISS and the vasa recta. Below, figure 6 outlines the movement of filtrate through the loop of Henle. [4]
Reabsorption and Secretion in the Distal Convoluted Tubule
Reabsorption in the distal convoluted tubule (DCT) is influenced by aldosterone, a hormone that increases the amount of Na+/K+ ATPase in the basal membrane of the DCT and collecting duct. The movement of sodium out of the lumen of the collecting duct creates a negative charge that promotes the movement of chloride out of the lumen into the interstitial space by a paracellular route across tight junctions. Peritubular capillaries receive the solutes and water and return them to circulation.
Cells of the DCT also recover calcium from the filtrate. Parathyroid hormone, once bound to its receptors in the DCT, induces the insertion of calcium channels on its luminal surface. As sodium is pumped out of the cell, the resulting electrochemical gradient attracts calcium into the cell. In addition, calcitriol, the active form of vitamin D, induces the production of calcium-binding proteins that transport calcium into the cell. Any calcium not reabsorbed at this point is lost in the urine. For more information on these hormones, go to the section titled “Hormonal Regulation“.
Collecting Ducts and the Recovery of Water
In the collecting ducts, there are two distinct types of cells. A principle cell, that possesses channels for the recovery or loss of sodium and potassium, and intercalated cells that secrete or absorb acid or bicarbonate.
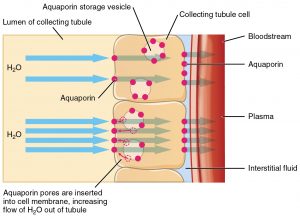
The regulation of urine volume and osmolarity are two major functions of the collecting ducts. By varying the amount of water that is recovered, the collecting ducts play a role in maintaining the body’s normal osmolarity. If the blood becomes hyperosmotic, the collecting ducts recover more water to dilute the blood; if the blood becomes hypoosmotic, the collecting ducts recover less water, leading to increased concentration of the blood. This function is regulated by antidiuretic hormone (ADH).
When stimulated by ADH, aquaporin channels are inserted into the apical membrane of principal cells. As the ducts descend through the medulla, the osmolarity surrounding them increases due to the countercurrent system. The aquaporin channels will osmotically pull water from the collecting duct into the surrounding interstitial space and the capillaries; this will concentrate the urine, as shown below in figure 7. Conversely, when ADH is not present, the limited aquaporin channels recover less water, making the urine more dilute.
Intercalated cells play significant roles in regulating blood pH. Intercalated cells reabsorb potassium and bicarbonate while secreting hydrogen. This function lowers the acidity of the plasma while increasing the acidity of the urine. The effects of hormones are explained more in-depth in the “Hormonal Regulation” section of the kidney unit.
The Countercurrent Multiplier System
The ascending limb actively reabsorbs salts like NaCl into the interstitial space (ISS) while the collecting ducts actively pump urea into the ISS space. This results in the recovery of salts into the circulation via the vasa recta and creates a high osmolar environment in the depths of the medulla.
The term countercurrent multiplier system comes from the proximity of the descending and ascending loops of the nephron as their fluid flows in opposite directions or in opposite currents. The multiplier term is due to the action of solute pumps that increase the concentrations of urea and sodium deep in the medulla. The net result of the countercurrent multiplier system is the recovery of both water and sodium in circulation.
In the vasa recta, blood flows at a rate that maintains the countercurrent multiplier system. The blood flows slowly through the capillaries to allow enough time for the exchange of nutrients and wastes. Additionally, the slow movement of blood through the vasa recta allows water to pass through without causing the vessels to swell or burst. It is also important to note, that if the flow through these capillaries was too rapid, the flow would remove too much sodium and urea which would destroy the osmolar gradient that is necessary for the reabsorption of solutes and water. The below videos give a good overview of the countercurrent multiplier system and how it is maintained.
Remember, the kidney works because the nephron is a loop to create a concentration gradient in medullary space to drive the movement of water and ions for reabsorption. Keep in mind moving forward that the countercurrent theory and the osmotic gradient in the medullary space are essential to understanding the effects of antidiuretic hormone on the distal tubule and collecting duct, which is a major topic in this unit.
Osmotic Gradient in the Medullary Space
The countercurrent multiplication theory, as discussed above, is the process of using energy to generate an osmotic gradient in the medullary space that drives reabsorption of water and solutes from the fluid in the tubule of the nephron into the blood. The loops of Henle in juxtamedullary nephrons are largely responsible for developing the osmotic gradients that are needed to concentrate urine. The following diagrams show how sodium and water move out of the loop of Henle and collecting duct based on concentrations gradients then move into the blood in the vasa recta for reabsorption. So, this shows how the osmotic gradient in the medullary space drives reabsorption in the kidney.
Now that you have learned about the countercurrent multiplier system and some of the hormones affecting osmoregulation, try these questions to test your knowledge and understanding!
Testing Your Knowledge
Thinking Beyond:
What would happen to the osmolarity of the filtrate with a decreased amount of antidiuretic hormone? Hint: Think about how ADH affects the permeability of the nephron!
Regulation of Reabsorption
The reabsorption of substances can be regulated at several locations along the nephron: the proximal tubule, the thick ascending limb of the Loop of Henle, the distal tubule, and the collecting duct. These mechanisms of regulation include both neural and hormonal regulation.
Neural Regulation
Direct sympathetic nervous system innervation along the entire tube of the nephron will increase sodium reabsorption. This increase in sodium in the blood will draw water to follow, therefore there will also be an increase in water reabsorption.
Hormonal Regulation
- Angiotensin II (AII) increases sodium reabsorption which will increase water reabsorption in the proximal tubule.
- Atrial natriuretic peptide (ANP) decreases sodium reabsorption which will decrease water reabsorption in the proximal tubule, distal tubule, and collecting duct.
- Aldosterone (ALDO) increases the number of symporters on the luminal side of the tubule and Na+/K+ ATPases on the ISS side which will increase sodium reabsorption and therefore increase water reabsorption in the thick ascending limb of the loop of Henle, distal tubule, and collecting duct.
- Antidiuretic hormone (ADH) increases the number of aquaporins on the luminal side of the tubule and the ISS side; which will increase water permeability, increasing the movement of water from the lumen to the ISS in both the distal tubule and collecting duct.
Recall that both the distal tubule and collecting duct are impermeable to water thus, reabsorption is highly dependent on the presence of hormones such as ADH. Without ADH, little sodium or water can be reabsorbed. The presence of ADH increases reabsorption retains water in the body and prevents the production of dilute urine.
Testing Your Knowledge
Clinical Application:
The importance of the kidneys in maintaining body fluid composition is clear when we consider the impact on the body when our kidneys start to fail. Diabetes insipidus is a rare disorder that causes you to feel very thirsty (despite drinking a lot), and to produce large amounts of dilute urine. The absence of which of the hormones discussed above would cause this?Hint: consider which hormone, whether increasing or decreasing, has a major influence on the reabsorption of water in the kidney.
For more information read about diabetes insipidus to help with this question.
Key Takeaways
Consider the following concepts to help guide your studies:
- At what locations in the nephron reabsorption and secretion occur.
- The permeability of each section in the nephron.
- The ramifications of hormones secreted by the body on the reabsorption and secretion of substances in the nephron.
Sub-chapter Quiz
The questions below can be used to assess your knowledge within this chapter. There are five multiple-choice questions that you should attempt without referring to your notes. The questions will provide you with responses to your answers to guide your studying but should not be used as your only resource.
Media Attributions
- Transport © BioRender is licensed under a CC BY (Attribution) license
- Locations of Secretion and Reabsorption in the Nephron © OpenStax adapted by Clare Thompson is licensed under a CC BY (Attribution) license
- Reabsorption © Brittany Emary is licensed under a CC BY (Attribution) license
- Private: substances reabsorbed and secreted by the PCT © OpenStax adapted by Clare Thompson is licensed under a CC BY (Attribution) license
- Private: Reabsorption of Bicarbonate from the PCT © OpenStax is licensed under a CC BY (Attribution) license
- Private: Loop of Henle © OpenStax is licensed under a CC0 (Creative Commons Zero) license
- 2710_Aquaporins-01 © OpenStax is licensed under a CC BY (Attribution) license
- Private: Countercurrent Multiplier System © OpenStax is licensed under a CC BY (Attribution) license
- Osmotic_Gradient © Brittany Emary is licensed under a CC BY (Attribution) license
- Vasa_Recta 2 © Brittany Emary is licensed under a CC BY (Attribution) license
- 25.6 Tubular Reabsorption - Anatomy and Physiology. OpenStax. (2013, April 25). ↵
- Animals at the extremes: The desert environment. OpenLearn. (2012). ↵
- Zacchia M, Capolongo G, Rinaldi L, Capasso G. The importance of the thick ascending limb of Henle’s loop in renal physiology and pathophysiology. Int J Nephrol Renovasc Dis. 2018;11:81-92 ↵
- Zacchia M, Capolongo G, Rinaldi L, Capasso G. The importance of the thick ascending limb of Henle’s loop in renal physiology and pathophysiology. Int J Nephrol Renovasc Dis. 2018;11:81-92 ↵
The process of removing a substance out of the bloodstream and into the urine.
The movement of molecules across a cell membrane against the concentration gradient (from low concentration to high concentration), which requires the use of energy.
A mechanism of transport that moves substances from an area of high to low concentration. No energy is needed.
A transportation mechanism that moves a substance down its concentration gradient. Requires specific membrane receptors or channel proteins for movement.
A carrier protein that transports two different molecules in the same direction across the cell membrane.
A carrier protein that transports two different molecules in opposite directions across the cell membrane.
A form of active transport across a cell membrane where a carrier protein couples the movement of a substance with its concentration gradient to the movement of another substance against its concentration gradient.
A hormone that is released from the posterior pituitary gland in response to low blood pressure. ADH increases water reabsorption in the kidney, which increases blood volume, and decreases urine excretion.
The interstitial space is a fluid-filled space that allows the free movement of ions, also referred to as interstitial fluid.
Dense network of capillaries and the site where kidney filtration begins.
The efferent arterioles that exit the glomerulus and become tiny blood vessels.
The function of the tubular network of the nephron is to discern nutrients from wastes and selectively replenish the blood with the water, salts, and nutrients that entered the filtrate.
Blood vessels that surround the loop of Henle.
In terms of kidney physiology, reabsorption is when the kidney removes water and solutes from the nephron and returns them to circulation.
The surface of an epithelial cell that is exposed to the body cavity or the exterior surface of an organ.
The surface facing the connective tissue base to which the cell attaches (basement membrane) or the cell membrane closest to the basement membrane.
An intermediate in cellular metabolism (HCO3-).
An enzyme present in the RBC that catalyzes the stripping of carbon dioxide from bicarbonate.
Proteins that allow for the movement of water across the hydrophobic lipid bilayer membrane.
A part of the nephron where water and solute reabsorption takes place.
The solute concentration of one solution is greater than another.
Transport of solutes by a cell through a cell.
The concentration of a solution.
A solution with a lesser concentration than another.
A very twisted tubule that is formed by simple cuboidal epithelium, the DCT responds to hormonal signals that regulate urine composition.
A solution with a higher concentration of solutes than another solution.
Leaky tight junctions are found between the cells of the ascending limb of the loop of Henle, where they allow the movement of certain solutes.
A hormone that is released from the adrenal cortex in response to angiotensin II or in direct response to an increased plasma K+ concentration. It promotes Na+ reabsorption by the nephron, promoting the retention of water.
A hormone secreted by the parathyroid glands that plays a role in regulating blood calcium concentration.
The active form of vitamin D.
Found in the collecting duct, these cells possess channels for the recovery or loss of sodium and potassium.
Found in the collecting duct and play a significant role in regulating blood pH. Intercalated cells reabsorb K+ and HCO3- while secreting H+.
Collects the filtrate from several nephrons for final modifications. The CD is continuous with the nephron but is not technically considered to be a part of the nephron.
A potent vasoconstrictor that plays an immediate role in the regulation of blood pressure.
A peptide hormone released from the heart that promotes the excretion of water and sodium by reducing the function of ALDO, ADH, and renin.