Hormonal Regulation
Learning Outcomes
In this section you will learn…
- The renin-angiotensin-aldosterone system.
- The interactions between different hormones.
- The stimuli for the release of hormones that regulate fluid volume.
- The effects of fluid regulating hormones.
The Renin-Angiotensin-Aldosterone-System
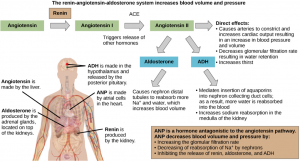
The renin-angiotensin-aldosterone-system, or RAAS for short, is a complex hormonal regulator of blood volume and pressure which influences cardiac output and arterial pressure. Many endocrine hormones are involved in the RAAS, illustrated in figure 1. This system proceeds through several steps to produce angiotensin II, which acts to stabilize blood pressure and volume. As the name implies, there are three important components to this system: 1) renin, 2) angiotensin, and 3) aldosterone.
Renin is secreted by a part of the juxtaglomerular complex and is produced by the granular cells of the afferent and efferent arterioles. Thus, the kidneys control blood pressure and volume directly. Renin acts on angiotensinogen, which is made in the liver and converts it to angiotensin I. Angiotensin-converting enzyme (ACE) then converts angiotensin I to angiotensin II. Angiotensin II is a potent vasoconstrictor and as a result of this, raises blood pressure. It also triggers the release of aldosterone from the adrenal cortex, which in turn stimulates the renal tubules to reabsorb more sodium. Angiotensin II also triggers the release of antidiuretic hormone (ADH) from the hypothalamus, leading to water retention in the kidneys. It acts directly on the nephrons and decreases the glomerular filtration rate. [1]
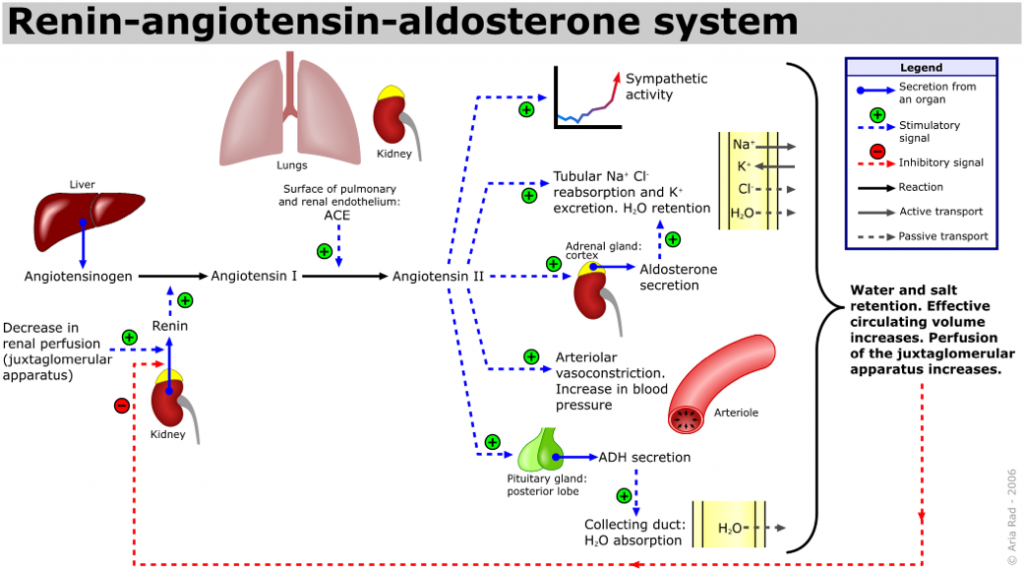
The diagram displayed in figure 2 will be extremely helpful when considering how the different hormones can be used as a tool to restore blood pressure. Take note of how a decrease in blood pressure will increase renin, angiotensin II, antidiuretic hormone, and aldosterone whereas an increase in blood pressure will increase atrial natriuretic peptide release, inhibiting the actions of the other hormones. Remember to fully work through these arguments to show how these hormones work to restore homeostasis.
Test Your Knowledge
Clinical Application:
Ever wonder how we control blood pressure when the renin-angiotensin-aldosterone system is too active? Many drugs interrupt different steps in this system to lower blood pressure. These drugs are one of the main ways to control high blood pressure, heart failure, kidney failure, and the harmful effects of diabetes. It is believed that angiotensin I may have some minor activity, but angiotensin II is the major bioactive product. If you were to design a drug to control the RAAS system, what step might you want to interrupt?Hint: Think about how you would stop angiotensin II.
The hormones of the RAAS, their secretion, and their subsequent actions will be discussed in depth in the following paragraphs. Keep in mind that while it is important to know the basics of each hormone and its subsequent impact on the body, it is also important to understand how these hormones work together to maintain homeostasis.
Renin
Renin is a proteolytic enzyme that is produced by the granular cells of the afferent arteriole at the juxtaglomerular apparatus (JGA). Once released, renin will combine with angiotensinogen to form active angiotensin I, which then will become active angiotensin II due to the conversion caused by the angiotensin-converting enzyme (ACE). Its release is stimulated by several factors. There is a direct relationship between renin release and blood pressure, with decreases in afferent arteriole pressure causing an increase in renin release. These afferent arterioles possess high-pressure baroreceptors that respond to changes in blood pressure and volume to stimulate renin release accordingly. There is also a direct relationship between renin release and sympathetic nervous system (SNS) activity, with increases in SNS activity increasing renin release. Finally, chemoreceptors in the distal convoluted tubule will respond to decreases in salt concentration at the macula densa, signalling to increase renin release. If you need a refresher on the macula densa, go back to the anatomy section from this chapter! These stimuli for the release of renin are described in the following video. [2]
Test Your Knowledge
Thinking Beyond:
Consider situations in which the body would trigger each stimulus for renin release. For example, would a change in whole-body mean arterial pressure trigger a local or a central response to release renin? Hint: Remember that changes in blood pressure will alter nervous system output!
Angiotensin II
Angiotensin II is a potent vasoconstrictor that is involved in maintaining homeostatic blood pressure. Its release is stimulated by decreases in blood pressure and it acts to return blood pressure to normal levels. It acts systemically to cause both vasoconstriction and venoconstriction, ultimately leading to the desired increase in blood pressure. But how does it act on the kidney?
Angiotensin II constricts both the afferent and efferent arterioles of the glomerulus. This reduces both glomerular filtration rate and renal blood flow, thereby limiting urine output and preserving blood volume. Its other direct effect on the kidney involves increasing sodium and water retention. Angiotensin II also stimulates the adrenal cortex to release aldosterone, which in turn acts on the kidneys to further increase sodium and fluid retention. In addition, angiotensin II stimulates the release of antidiuretic hormone (ADH) from the posterior pituitary which also causes an increase in sodium and fluid retention by the kidneys. Thirst centers within the brain are activated and this facilitates norepinephrine release from the sympathetic nerve endings and inhibits norepinephrine reuptake by nerve endings. The sympathetic adrenergic function is enhanced and in the end, this stimulates both cardiac hypertrophy and vascular hypertrophy. Figure 2, shown below, is a helpful tool to visualize the effects of angiotensin II on the body. [3]
Aldosterone
Aldosterone (ALDO) is released from the adrenal cortex in response to an increase in angiotensin II. Aldosterone release stimulates increased reabsorption of sodium and given that water follows sodium, this results in an increased reabsorption of water. This overall increase in fluid retention leads to an increase in blood pressure. Did you know that progesterone is structurally very similar to aldosterone? Because of this, progesterone is able to bind to aldosterone receptors stimulating sodium and fluid retention. This could explain the increase in fluid retention that occurs in menstruators during parts of their menstrual cycle in which progesterone levels are high. The following video is a useful summary of the RAAS. While it is not a fully fleshed explanation, it may help if you are struggling with the foundation of this system. [4] [5]
Angiotensin-Converting Enzyme
While angiotensin-converting enzyme (ACE) is not a hormone, it is incredibly important in the regulation of kidney function and therefore, blood pressure. ACE is an enzyme that is produced in the lungs and released into the systemic circulation. There, it finds its way to the kidney and binds to the surface of the afferent arteriole and glomerular endothelium. This is where it will convert angiotensin I into angiotensin II, which then goes on to promote an increase in blood pressure. [6]
Antidiuretic Hormone
Have you ever wondered why you feel dehydrated after having a few glasses of wine or beer? This is because alcohol is a diuretic that inhibits the release of antidiuretic hormone (ADH). This hormone is produced in the hypothalamus and is delivered to the posterior pituitary for storage and release. ADH controls the amount of water reabsorbed from the collecting ducts and tubules in the kidney. When osmoreceptors in the hypothalamus detect an increase in the concentration of blood plasma, the hypothalamus signals the release of ADH from the posterior pituitary into the bloodstream. ADH will also be released if the low-pressure baroreceptors in the body detect a decrease in blood volume or pressure. This will decrease the inhibition of ADH secreting cells in the posterior pituitary and promote its release. ADH acts on the body by changing the permeability of the nephron to water and causing systemic vasoconstrictor, as described in the following paragraphs.
ADH alters the permeability of the nephrons by stimulating the movement of aquaporin proteins into the apical cell membrane of principal cells of the collecting ducts. This results in an increase in the water permeability of these cells and, thus, a large increase in water passage from the urine through the walls of the collecting tubules, leading to more reabsorption of water into the bloodstream. When the blood plasma becomes less concentrated and the level of ADH decreases, aquaporins are removed from collecting tubule cell membranes, and the passage of water out of urine and into the blood decreases. The video below explains the movement of aquaporins to the apical side of the membrane in the collecting duct.
“How does ADH work?“by Macrophage. Co. is All Rights Reserved.
Did you know that antidiuretic hormone (ADH) is also called vasopressin? Early researchers found that in cases of unusually high secretion of ADH, the hormone caused vasoconstriction or vasopressor activity, hence the name. ADH causes the vasoconstriction of the afferent arterioles in the peripheral circulation reducing the flow of blood to the extremities and thereby increasing the blood supply to the core of the body. Only later were its antidiuretic properties identified. Synthetic ADH is still used occasionally to stem life-threatening esophagus bleeding in alcoholics due to its vasoconstrictive actions. [7] [8]
Test Your Knowledge
Real-Life Scenario:
Keep in mind that a decrease in blood volume will increase ADH release which eventually causes increases in water reabsorption and blood volume while decreasing plasma osmolarity. This change then decreases ADH release and will restart this cycle of receptors. How might the body work to combat this cycle? Hint: Think about the receptors involved and how their sensitivity might change in response to different stimuli!
Natriuretic Hormones
Natriuretic hormones are a peptide hormone group that counter the effects of the RAAS, acting to lower blood pressure. You may remember one natriuretic hormone in particular from your course notes, the atrial natriuretic peptide, or ANP. ANP is produced by the atria of the heart in response to the stimulus of the stretch receptors; which could be caused by an increase in blood pressure or volume. ANP and other members of this hormone group act to inhibit the release of aldosterone. Remember, aldosterone acts on the kidney to increase salt and fluid retention. Therefore, inhibiting its release would force sodium to remain in the filtrate and since water passively follows sodium, this will also increase fluid loss and an overall decrease in blood volume and pressure. In addition, ANP acts as a vasodilator on the afferent arteriole of the glomerulus while it vasoconstricts the efferent arteriole. This in turn increases glomerular filtration rate, leading to an increase in sodium and fluid lost in the urine. Finally, ANP acts to decrease the reabsorption of sodium in the distal convoluted tubule of the nephron. The flowchart in figure 3 is helpful in visualizing how ANP directly impedes the RAAS.
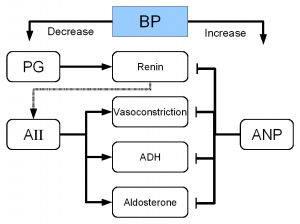
As you can see in the image above, ANP also inhibits the release of renin and antidiuretic hormone (ADH). By inhibiting the release of renin, it further interrupts the RAAS by preventing the activation of the system itself. In addition, by inhibiting the release of antidiuretic hormone, it further promotes diuresis by decreasing the nephron’s permeability to water preventing its reabsorption. [9]
Tips From Past Students
Remember: All of the effects of ANP will work to increase filtration and decrease reabsorption at the kidney. This will lead to an increase in the excretion of water which will decrease blood volume and blood pressure.
Did you know that there is also a B-type natriuretic peptide? This is abbreviated as BNP and it is produced in the ventricles of the heart. BNP is much less potent than ANP since its receptor affinity is lower. Since its effects are minute, it is theorized that BNP is useful in small tweaks in blood pressure regulation. [10]
This table summarizes the hormones that have been discussed thus far. This is helpful in understanding the mechanisms of the kidney and may be helpful to refer back to as you study. [11]
| Hormone | Where is it produced? | Function |
|---|---|---|
| Epinephrine and Norepinephrine | Adrenal medulla | Can decrease kidney function temporarily by vasoconstriction |
| Renin | Kidney nephrons | Increases blood pressure by acting on angiotensinogen |
| Angiotensin | Liver | Angiotensin II affects multiple processes and increases blood pressure |
| Aldosterone | Adrenal cortex | Prevents loss of sodium and water |
| Antidiuretic hormone | Hypothalamus (stored in the posterior pituitary) | Prevents water loss |
| Atrial natriuretic peptide | Heart atrium | Decreases blood pressure by acting as a vasodilator and increasing glomerular filtration rate; decreases sodium reabsorption in the kidneys |
Test Your Knowledge
Real-Life Scenario:
It is a sunny Monday morning and you have woken up late for class (oh no!) and have to run to campus to make it on time for your physiology lecture. As you are running, your heart is pumping faster and harder to circulate more blood to your muscles. As a result, your mean arterial pressure also rises. How does the kidney respond to this change, both locally and centrally? Hint: The local control of the kidney is doing its best to keep the glomerular filtration rate constant, but central control wants to solve the problem that altered this in the first place!
Endothelin
Endothelins are peptides that are produced by the endothelium of the renal blood vessels and the distal convoluted tubules. These are potent vasoconstrictors and their release is stimulated by angiotensin II, bradykinin, and epinephrine. Endothelins mainly affect those suffering from diabetic kidney disease, in which endothelin levels are chronically high. This leads to the chronic decrease of glomerular filtration rate, and the retention of sodium and water. This hormone is not explicitly discussed in HK*3810 and this information is here for your interest. [12]
Parathyroid Hormone
You may remember this peptide hormone from HK*2810, the parathyroid hormone (PTH). PTH is produced by the parathyroid glands as a result of a decrease in blood calcium levels. PTH acts on the proximal convoluted tubule where it stimulates the formation of calcitriol, the active form of vitamin D. In addition, PTH prevents the reabsorption of phosphate in the nephron which allows calcium levels in the blood to rise. [13]
Key Takeaways
Consider the following concepts to help guide your studies:
- The actions of each hormone discussed.
- How the body regulates kidney function locally.
- How the body regulates kidney function systemically.
- How the kidney can be used as a tool to fix systemic problems, such as a change in blood pressure.
Subchapter Quiz
The questions below can be used to assess your knowledge within this chapter. There are multiple-choice questions that you should attempt without referring to your notes. The questions will provide you with responses to your answers to guide your studying but should not be used as your only resource.
Media Attributions
- Private: Renin-Angiotensin-Aldosterone Effect on Osmoregulation © OER Commons is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- Private: Renin-Angiotensin-Aldosterone System © LumenLearning is licensed under a CC BY-SA (Attribution ShareAlike) license
- RenalHormoneRegulation © WikiMedia adapted by Ted D. Williams is licensed under a CC BY-SA (Attribution ShareAlike) license
- Rice University. (n.d.). Biology, Animal Structure and Function, Osmotic Regulation and Excretion, Hormonal Control of Osmoregulatory Functions. OER Commons. ↵
- 25.8 Endocrine Regulation of Kidney Function - Anatomy and Physiology. OpenStax. (2013, April 25). ↵
- 25.8 Endocrine Regulation of Kidney Function - Anatomy and Physiology. OpenStax. (2013, April 25). ↵
- Renin-Angiotensin-Aldosterone System. Image for Cardiovascular Physiology Concepts, Richard E Klabunde PhD. (2016). ↵
- 25.8 Endocrine Regulation of Kidney Function - Anatomy and Physiology. OpenStax. (2013, April 25). ↵
- 25.8 Endocrine Regulation of Kidney Function - Anatomy and Physiology. OpenStax. (2013, April 25). ↵
- 25.8 Endocrine Regulation of Kidney Function - Anatomy and Physiology. OpenStax. (2013, April 25). ↵
- 26.2 Water Balance - Anatomy and Physiology. OpenStax. (2013, April 25). ↵
- 25.8 Endocrine Regulation of Kidney Function - Anatomy and Physiology. OpenStax. (2013, April 25). ↵
- Rice University. (n.d.). Biology, Animal Structure and Function, Osmotic Regulation and Excretion, Hormonal Control of Osmoregulatory Functions. OER Commons. ↵
- Rice University. (n.d.). Biology, Animal Structure and Function, Osmotic Regulation and Excretion, Hormonal Control of Osmoregulatory Functions. OER Commons. ↵
- 25.8 Endocrine Regulation of Kidney Function - Anatomy and Physiology. OpenStax. (2013, April 25). ↵
- 25.8 Endocrine Regulation of Kidney Function - Anatomy and Physiology. OpenStax. (2013, April 25). ↵
An enzyme produced by the granular cells of the afferent arteriole at the JGA. It enzymatically converts angiotensinogen to angiotensin I.
A hormone that is released from the adrenal cortex in response to angiotensin II or in direct response to an increased plasma K+ concentration. It promotes Na+ reabsorption by the nephron, promoting the retention of water.
A potent vasoconstrictor that plays an immediate role in the regulation of blood pressure.
A hormone that is released from the posterior pituitary gland in response to low blood pressure. ADH increases water reabsorption in the kidney, which increases blood volume, and decreases urine excretion.
A structure formed by the distal convoluted tubule and the glomerular afferent arterioles. Involved in the regulation of blood pressure and GFR.
The circuit that provides oxygenated blood to the entire body, except the lungs (blood moving to and from the lungs is considered pulmonary circulation).
Contraction of smooth muscle cells and the tightening of blood vessels. This will allow for less blood flow through the vasculature.
This enzyme is not a hormone but it is functionally important in regulating systemic blood pressure and kidney function. It enzymatically converts inactive angiotensin I to active angiotensin II.
Small portion of the brain that regulates metabolic processes, serving as a link between endocrine and nervous systems via the pituitary gland.
Pituitary gland lobe that does not produce its own hormones. Hormones synthesized in the hypothalamus reach the posterior pituitary where they are secreted in systemic circulation.
Proteins that allow for the movement of water across the hydrophobic lipid bilayer membrane.
A peptide hormone released from the heart that promotes the excretion of water and sodium by reducing the function of ALDO, ADH, and renin.
A hormone secreted by the parathyroid glands that plays a role in regulating blood calcium concentration.
The active form of vitamin D.

