Structure and Motility
The gastrointestinal tract, as you will soon see, is a highly integrated system utilized for the digestion and absorption of food constituents to provide us with nutrients essential for basic human functions. This chapter will provide a summary of the structure and functions of the gastrointestinal tract.
Learning Outcomes
In this section you will learn…
- The overall structure of the gastrointestinal tract.
- Movement/motility of foodstuffs and the concept of directionality.
- Electrophysiology and neural innervations within the wall of the gastrointestinal tract.
The gastrointestinal tract is a specialized tube for the processing of foods. It contains functional compartments that are separated by sphincters. It is important to understand the arrangement of the organs and the sphincters in order to understand how the GIT functions.
General Anatomy
As is the case with all body systems, the digestive system does not work in isolation; it functions cooperatively with the other systems of the body. Consider for example, the interrelationship between the digestive and cardiovascular systems. Arteries supply the digestive organs with oxygen and processed nutrients, and veins drain the digestive tract. These intestinal veins, constituting the hepatic portal system, are unique; they do not return blood directly to the heart. Rather, this blood is diverted to the liver where its nutrients are off-loaded for processing before blood completes its circuit back to the heart. At the same time, the digestive system provides nutrients to the heart muscle and vascular tissue to support their functioning.
The interrelationship of the digestive and endocrine systems is also critical. Hormones secreted by several endocrine glands, as well as endocrine cells of the pancreas, the stomach, and the small intestine, contribute to the control of digestion and nutrient metabolism. In turn, the digestive system provides the nutrients to fuel endocrine function. [1]
Functions of the Digestive Organs
In its simplest form, the digestive system is a long tube connecting the mouth and the anus. The goal of this tube is to break down large macromolecules into smaller molecules (amino acids, fatty acids and glucose) which can then be absorbed and function throughout the body.
Digestive system components can be broken down into two main parts: the alimentary tract and accessory organs. The alimentary tract is composed of the mouth, pharynx, esophagus, stomach, small and large intestines, rectum and anus. Associated with these organs are the accessory organs: salivary glands, liver, gallbladder and pancreas. Take a look Table 1: Digestive system components and functions, to learn more about the major functions of each organ in the digestive system. Notice that the digestive system is made up of the gastrointestinal tract in addition to other components. The GIT consists of the hollow organs connected to one another: mouth, esophagus, stomach, small intestines, large intestines, anus. These are outside the body. The liver, pancreas and gall bladder are solid organs that are included along with the GIT in the digestive system that are inside the body. When you are studying, continually ask yourself, “Am I inside or outside the body right now?” as it will help you to center yourself in the body. [2]
| Organ | Major Functions | Other Functions |
|---|---|---|
| Mouth |
|
|
| Pharynx |
|
|
| Esophagus | Upper Esophageal Sphincter:
Esophagus
Lower Esophageal Sphincter:
|
|
| Stomach |
|
|
| Small Intestine |
|
|
| Large Intestine |
|
|
|
Accessory Organs |
Liver:
Gallbladder:
Pancreas:
|
|
Now that you have a basic understanding of the various organs that make up our GI tract, let’s test your knowledge of their functions!
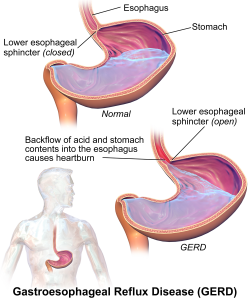
Ever wonder what causes heartburn? Gastrointestinal Reflux disease a.k.a GERD is a disease that affects the lower esophageal sphincter. In this condition, the sphincter is not effective at preventing backflow. This causes stomach acids to travel up into the esophagus and causes heartburn.
Directionality
Our GIT functions such that food flows in one direction to allow for digestion, absorption and subsequent excretion of waste products. This section describes the concept of directionality and movement of food through the digestive tube.
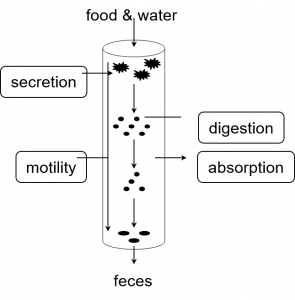
One tricky aspect of the gastrointestinal tract content to grasp is the concept of directionality! The whole purpose of the gastrointestinal tract is to move foreign foodstuffs from the “outside” of the body inwards. This movement happens along with many other processes, such as digestion, secretion, motility, excretion, etc.
Understanding what is considered “outside” of the body, and what is “inside” when discussing the gastrointestinal tract can be confusing to think about but is important to wrap your head around. The following video: Epithelial Tissue 4 Functions by Wendy Riggs will provide you with a simplification of our gastrointestinal tract including a great analogy to help you understand this idea by watching from 0:50-2:56. We will also take a look at the processes that allow substances to move in and out of the body. The video from 4:37-6:25 is beneficial in explaining these concepts as well.
As mentioned above, there are many processes happening simultaneously to make digestion and absorption possible.
Lets to take a closer look at what epithelial tissue really is. On a smaller scale, epithelial cells also have directionality! They are asymmetrical cells, which makes much of the absorption and secretion they carry out possible! The following video: Epithelial Tissue 3 – Basic characteristics by Wendy Riggs describes the general characteristics of epithelial cells. Watch from 7:48-10:21. This clip addresses only the directionality of the epithelial cells, but if you’re curious, watch the rest of the video – it’s valuable information!
Cross Section of the GIT
The GIT is composed of layers that all play important roles in the proper functioning of the GIT. The gastrointestinal tract is composed of four main layers: serosa, muscularis, submucosa and mucosa. Take a look at the following video: Digestive System Part 1: Crash Course A&P #33 by CrashCourse which gives a brief overview of the layers of the GIT as well as each of their roles by watching 4:07-6:02. Please note that this learning object is beyond course level but may help foster a deeper understanding.
Memorizing each layer is important as you may need to refer to them when answering a question (you will never need to label a diagram). However, you should also have a good understanding of the various components. Think about it like this: the mucosa layer is the innermost layer, what’s its purpose? It secretes mucous to protect the GIT from the digestive fluids present. Without it, there could be severe damage to the inner lining of our GIT. Thinking like this may help you get less caught up in blindly memorizing, rather it forces you to engage with the content.
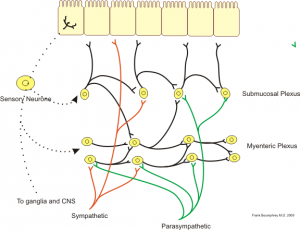
The Enteric Nervous System
The GIT needs to be innervated in order for digestion to occur which can happen both centrally and locally. The gut is highly innervated, both centrally and locally. From the central nervous system (CNS), the gut is innervated by the autonomic nervous system(ANS), which contains the sympathetic nervous system and parasympathetic nervous systems (SNS and PNS respectively). Locally, we have the enteric nervous system, a network of nervous tissue in the lining of the GIT, in the myenteric and submucosal plexuses. Don’t get caught up in memorizing the layers of the tube as seen in figure 4 we’re just showing this to put the location of the plexuses in context.
Inputs and Outputs of the GIT Neuronal Network
Outputs include specialized receptors (sensory neurons) at the level of the GIT lumen that can send information to either the central nervous system (CNS) or the enteric nervous system (ENS). These are known as long/central reflexes and short/local reflexes, respectively.
Inputs include SNS, PNS and ENS synapsing onto one another, and the enterocytes directly. The SNS, being the “fight or flight” system inhibits digestive processes. Conversely, PNS (the “rest and digest” system) promotes digestive processes. By virtue of their location, the myenteric and submucosal plexuses serve different purposes. Between two layers of muscle, the myenteric plexus primarily causes muscular contraction in the gut. The submucosal plexus, which lies right beneath the enterocytes, promotes secretions from the GIT.
Can you identify these pathways in figure 5 below?
Try the following question below to test your knowledge![4] [5]
Tips From Past Students
Keep in mind, all of the neurons found in the ENS are no different from those you’ve learned about in previous units! They all follow the same principles; they depolarize from a stimulus, causing an action potential, which is then propagated to other neurons. The ENS – just like the CNS – has sensory, motor and interneurons! Can you see how this all fits together?
Electrophysiology of GIT
Action potentials operate uniquely in the digestive tract and so this section will discuss slow waves and spike potentials. Normal gastrointestinal motility results from coordinated contractions of smooth muscle, which in turn derive from two basic patterns of electrical activity across the membranes of smooth muscle cells – slow waves and spike potentials.
Tips From Past Students
Focus on understanding the difference between slow waves, spike potentials, and how they come about. Integration is also very important, so consider how all of this would be applied on a large scale in the body.
The resting membrane potential of smooth muscle cells is between −50mV (millivolt) and −60 mV. In contrast to nerves and other types of muscle cells, the membrane potential of smooth muscle cells fluctuates spontaneously. Because the cells are electrically coupled, these fluctuations in membrane potential spread to nearby muscle, resulting in what is called “slow waves” – waves of partial depolarization in smooth muscle that sweep along the digestive tube for long distances. These partial depolarizations are equivalent to fluctuations in membrane potential of 5mV to 15 mV. The frequency of slow waves depends on the section of the digestive tube – in the small intestine, they occur 10 to 20 times per minute and in the stomach and large intestine 3 to 8 times per minute. Slow wave activity appears to be a property intrinsic to smooth muscle and not dependent on nervous stimuli. Importantly, slow waves are not action potentials and by themselves do not elicit contractions.
Spike potentials are true action potentials that elicit muscle contraction. They result when a slow wave passes over an area of smooth muscle that has been partially depolarized by exposure to neurotransmitters released in their vicinity by neurons of the enteric nervous system. The neurotransmitters are released in response to a variety of local stimuli, including distension of the wall of the digestive tube (which happens when foodstuffs enter). [6]
Taking a look at the image below we see the partial depolarization (5mV to 15 mV) that occurs below the threshold potential line. These sections of depolarization are known are slow waves and by themselves do not elicit muscle contraction as depicted below. Spike potentials occur at the crest of slow waves and are the true action potentials that are seen above the threshold line which elicit muscle contraction.
One can now step back and understand how electrophysiology helps move food. Consider what happens when foodstuff enters the small intestine. First, the foodstuff distends the gut, stretching its walls. Next, the stretching stimulates nerves in the wall of the gut to release neurotransmitters into the smooth muscle at the site of distension – the membrane potential of that section of muscle becomes “more depolarized.”. When a slow wave passes over this area of sensitized smooth muscle, spike potentials form and contraction results. The contraction moves around and along the gut in a coordinated manner because the muscle cells are electrically coupled through gap junctions.
Tips From Past Students
- Slow waves ≠ Action potential
- Slow wave + a stimulus (ie. stretch from food) at the site where a slow wave is passing over = Action Potential
- A slow wave alone is insufficient and will not lead to an action potential and the resulting muscle tension
Gastrointestinal Mobility
Propulsion and churning motions in the digestive tract are two very important terms that help us understand the movement of foodstuffs through the digestive tract. Two fundamental patterns of motility are conducted by the digestive tube: Propulsion and Segmental Contractions (Mixing).
Ever wonder why your stomach gurgles? When your stomach “gurgles” in between meals, this is due to intestinal muscle contractions that are working to propel foods!
Propulsion
Foodstuffs must be propelled along the length of the digestive tube in order to be subjected to the sequential series of processing involved in disassembly and absorption. Propulsion occurs via peristalsis, which is shown below, with the ultimate goal of moving food through the GI tract. Muscle contraction occurs and moves the foodstuffs directionally down the GIT towards the anus. Remember when you were a kid and moved your clenched fist up a yogurt tube to get everything out? It’s like that but everything is being pushed down.
Mixing
Ingested materials also need to be mixed with digestive enzymes, and put in contact with epithelial cells that absorb nutrients. Without this, you would expect very poor digestion and absorption. Segmentation contractions are a common type of mixing motility seen especially in the small intestine. Segmental rings mix the foodstuffs by alternating contraction and relaxation of the longitudinal muscles in the wall of the gut. If you’re having trouble visualizing this, think about taking a bag of frozen berries out of the freezer, and how you squish the bag to break up the contents before you use it!


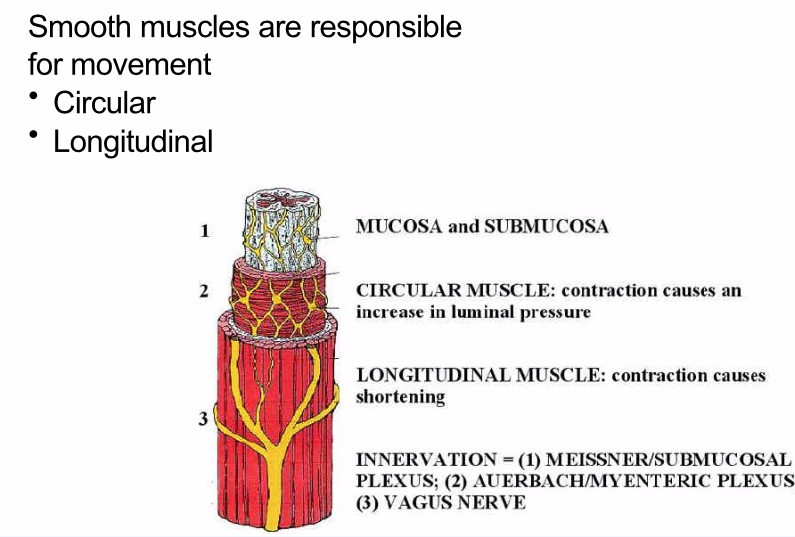
Except for the first section of the esophagus, all the muscle in the wall of the digestive tube is smooth muscle. Smooth muscle fibers are arranged in intertwined, rather indistinct bundles, aligned in most areas of the tube in circular and longitudinal layers. Individual smooth muscle fibers are connected to neighbouring smooth muscle cells by gap junctions, which allow these cells to be electrically coupled. The importance of this electrical coupling is that when an area of smooth muscle becomes depolarized, that depolarization spreads outward through adjacent sections of smooth muscle – this results in a well-coordinated contraction of, for example, an entire ring of circular smooth muscle. Without electrical coupling through gap junctions, one would imagine that you would see contraction only of patches of circular or longitudinal muscle, which would have little effect on propulsion or mixing of foodstuffs. [7]
Take a look at figure 11 below which outlines the circular and longitudinal smooth muscles that exist in the small intestine and aid with the movement and mixing of food. Although this diagram is of the small intestine, circular and longitudinal muscles are found throughout the rest of the GI tract. They are vital for the movement of food from the esophagus to the anus.
Try the following question below to test your knowledge!
Test Your Knowledge
Real-Life Scenario:
You are eating at the Gryphon Grill and have just swallowed a mouthful of hamburger. The bolus of food is now in your esophagus, describe the membrane potential before the bolus of food entered the esophagus. What is the process of increasing motility of this bolus of food down the esophagus? What type of movement is causing the bolus of food to travel down the esophagus? Hint: Think about the concepts covered above regarding anatomy and motility.
Villi Anatomy
The small intestine, aka nutrient absorption site, has a remarkably great surface area all thanks to villi and microvilli. Villi are microscopic finger-like pieces of tissue called villi. These individual epithelial cells also have finger-like projections known as microvilli. The function of the villi, and the microvilli is to increase the amount of surface area available for the absorption of nutrients. [8]
The small intestine is the site of nutrient absorption. Processes here are facilitated by specialized epithelial cells. These cells line the lumen of the small intestine. Some are specialized for absorption while others are tasked with secretion to aid in digestion. The key of these cells is their massive surface area which maximizes the interaction of foodstuffs with the epithelial layer.
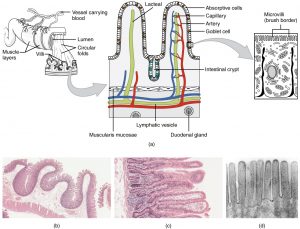
The ultimate purpose of the small intestine is to absorb foodstuffs, consider how increased surface area helps with this goal. If there are more places for chyme to come into contact with the epithelial cells, these cells have more opportunity to complete these functions. It can be helpful to think of villi as little nets, that reach out and catch the foodstuffs, increasing absorption.
Key Takeaways
Consider the following concepts to help guide your studies:
- The organs that make up the GI tract and their functions.
- How smooth muscles allow for movement/motility of foodstuffs.
- The difference between slow waves and spike potentials.
- How gastrointestinal mobility allows for both movement and mixing of food.
Subchapter Quiz
The questions below can be used to assess your knowledge within this chapter. There are multiple-choice questions that you should attempt without referring to your notes. The questions will provide you with responses to your answers to guide your studying but should not be used as your only resource.
Media Attributions
- GI system diagram © Docsity is licensed under a All Rights Reserved license
- GERD © Bruce Blaus is licensed under a CC BY-SA (Attribution ShareAlike) license
- Basic Processes of the GI Tract © John Williams, M.D., Ph.D. is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- GI Nerves © Richard Bowen is licensed under a All Rights Reserved license
- Neural_control_gut © Boumphreyfr is licensed under a CC BY-SA (Attribution ShareAlike) license
- Slow Waves © Richard Bowen is licensed under a All Rights Reserved license
- Peristalsis © Deepanakar Parmar is licensed under a All Rights Reserved license
- Peristalsis © Richard Bowen is licensed under a All Rights Reserved license
- Segmental Contraction © Richard Bowen is licensed under a All Rights Reserved license
- The smooth muscles responsible for small intestine movement is licensed under a CC BY-SA (Attribution ShareAlike) license
- Microvilli animation © Thomas Schwenke is licensed under a All Rights Reserved license
- Histology of the Small Intestine © Donna Browne is licensed under a CC BY (Attribution) license
- Browne, D. (n.d.). Digestive System Module 1: Overview of the Digestive System. Retrieved April 10, 2021, from https://cnx.org/contents/3xzxwV_7@1.1:Z66DGhlA@1/Digestive-System-Module-1-Overview-of-the-Digestive-System ↵
- Regions of the digestive system. Retrieved April 10, 2021, from https://training.seer.cancer.gov/anatomy/digestive/regions/ ↵
- Functions of the Digestive Organs ↵
- 23.2 digestive system processes and regulation - anatomy and physiology. (n.d.). Retrieved April 10, 2021, from https://openstax.org/books/anatomy-and-physiology/pages/23-2-digestive-system-processes-and-regulation ↵
- Bowen, R. (n.d.). The Enteric nervous system. Retrieved April 10, 2021, from http://www.vivo.colostate.edu/hbooks/pathphys/digestion/basics/gi_nervous.html# ↵
- Bowen, R. Electrophysiology of gastrointestinal smooth muscle. Retrieved April 10, 2021, from http://www.vivo.colostate.edu/hbooks/pathphys/digestion/basics/slowwaves.html ↵
- Bowen, R. (n.d.). Gastrointestinal motility and smooth muscle. Retrieved April 10, 2021, from http://www.vivo.colostate.edu/hbooks/pathphys/digestion/basics/gi_motility.html ↵
- Boundless. Boundless anatomy and physiology. Retrieved April 10, 2021, from https://courses.lumenlearning.com/boundless-ap/chapter/absorption/ ↵
Circular muscle that opens or closes the end of a tube.
Breaking food into pieces that are smaller and more nutrient accessible.
Chemical secretions that break down small food particles into their basic nutrient components.
Muscle that is controlled in a voluntary manner.
Muscle contractions done by conscious choice.
Muscle contractions that are autonomous, done without thinking.
Secreted from mucous glands, an aqueous substance that coats mucous membranes.
Partially digested/partially fluid food particles mixed with various gastric secretions.
Projections that stem from the inner lining of the small intestine to increase surface area.
Projections from the epithelial cells lining the villi to increase surface area.
Similar to mechanical digestion, it involves breaking food into pieces that are smaller and more nutrient accessible.
Bacteria that resides in the intestines.
The most prominent part of bile, the salts work to help emulsify fat.
The mixing of substances that typically do not combine easily due to their chemical properties.
The nerves of the brain and spinal cord.
Involuntary regulation of glands and organs in the body.
Commonly known for “rest and digest” of the body, this system promotes digestion and relaxation, and decreases heart rate.
Nervous tissue located between the circular and longitudinal muscles.
Nervous tissue located between the submucosa and circular muscle.
The small fluctuation of membrane potential due to the movement of ions.
An action potential generated from the combination of a slow wave and a stimuli.
Pushing something in one direction.
The contraction of a muscle pushing contents of a tube in a linear fashion.

