Kidney Vasculature
As you have learned in lectures, the term renal is used interchangeably with structures related to the kidney. Renal arteries carry the oxygenated blood from the heart to the kidneys. Remember, afferent arterioles bring blood to the glomerulus while efferent arterioles take blood away from the glomerulus. In this subchapter, we will see how the vasculature of the kidney can be controlled through autoregulation and radius resistance.
Learning Outcomes
In this section you will learn…
- Identify the major vasculature associated with the kidney and trace the path of blood through the kidney.
- Understand the mechanisms to control and regulate the kidney vasculature.
Nephron Blood Flow
The figure below depicts the order of blood flow through the kidney and the major blood vessels associated with this. The important takeaway here is the location of the afferent and efferent arterioles in relation to the glomerulus and the peritubular capillaries.
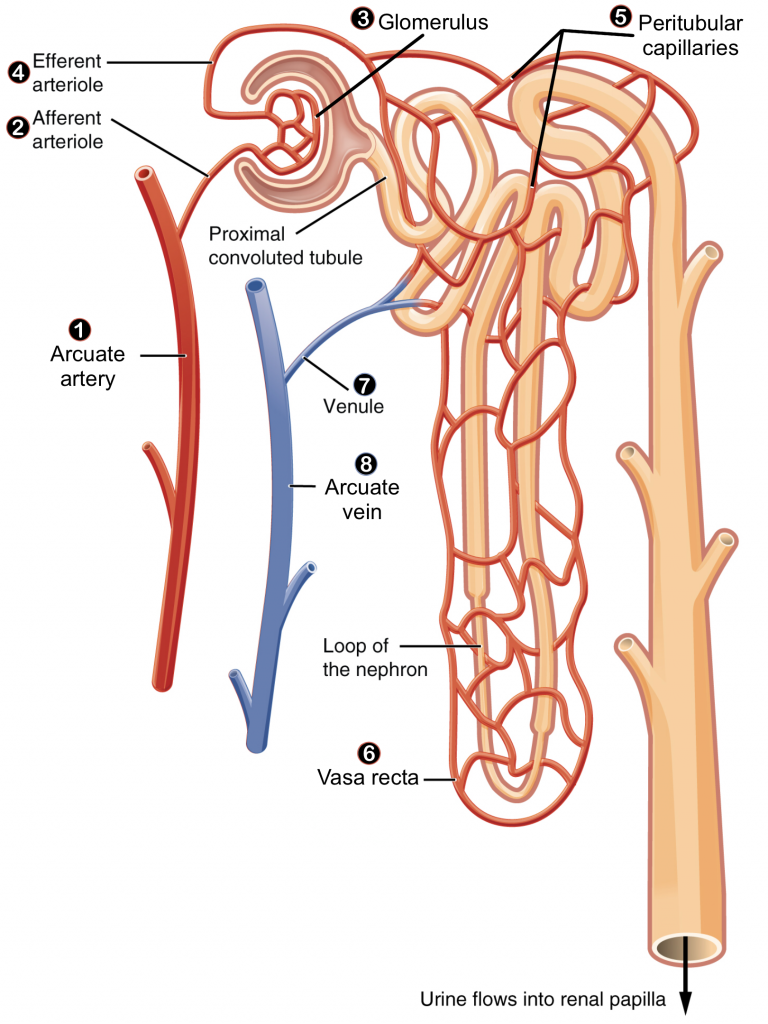
Surrounding the tube of the nephron is the vasculature of the kidney that permits blood flow through the kidney:[1]
- Blood flows from the arcuate artery into the afferent arteriole which brings blood into the glomerulus (a capillary bed)
- The efferent arteriole carries blood out of the glomerulus and becomes the peritubular capillaries that surround the nephron
- Downstream of the peritubular capillaries is the arcuate vein
Tips From Past Students
Remember when we talked about the difference between a cortical nephron and a juxtamedullary nephron?
The peritubular capillaries are associated with both types of nephrons. However, the vasa recta are only associated with a juxtamedullary nephron as it is the extension of the peritubular capillaries that follows the Loop of Henle down into the medullary space.
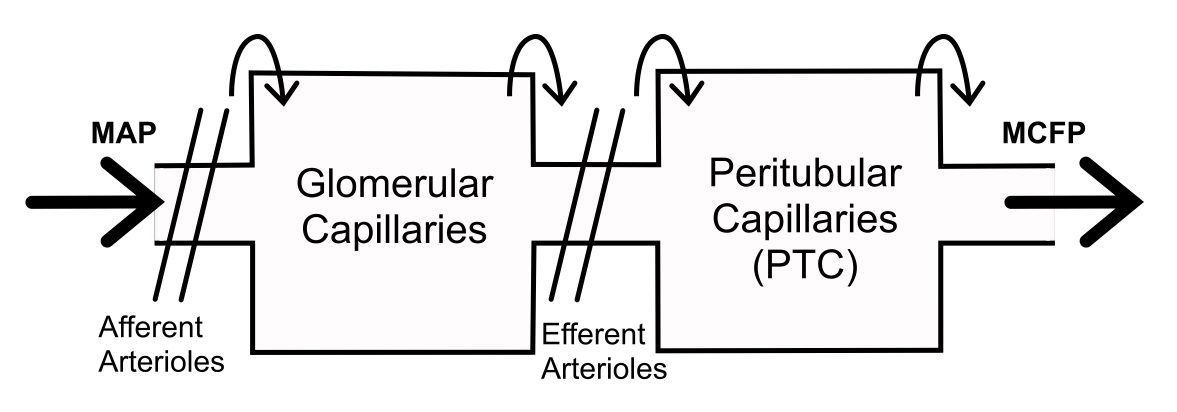
Take note of how blood flow through the kidney is different from blood flow in other tissues as the kidney has two sets of arterioles. Both the afferent and efferent arterioles can relax and contract to allow for control of volume into and out of the glomerular capillary bed. Volume into the capillary bed depends on afferent resistance and volume out of the capillary bed depends on efferent resistance. The resistance at both of these arterioles allows for lots of control over the volume and pressure in the glomerulus to help with filtering at the kidney.
Here is an example: if there is vasoconstriction of the afferent arterioles then there is decreased blood volume flowing into the glomerular capillary bed, therefore, there is reduced volume inside of the capillary bed which results in a decreased pressure in the glomerulus (PG).
Tips From Past Students
Always practice going through the opposite arguments (hint: what happens when there is vasoconstriction of the afferent arterioles?)
Control of the Kidney Vasculature
There are 2 mechanisms of control over the vasculature at the level of the kidney that we will focus on:
- Autoregulation
- Control of the radius of afferent and efferent arterioles
Autoregulation
The kidneys are very effective at regulating the rate of blood flow over a wide range of blood pressures. Blood pressure is decreased while relaxed or sleeping and increased while exercising. Yet, despite these changes, filtration rate and blood flow through the kidney will change very little. This is due to an autoregulatory mechanism that operates without outside influence known as the myogenic response.
The following formula helps to understand GFR and how various factors affect it. In this situation, Q is renal blood flow in the kidney, R is the resistance and P1 – P 2 represents the change in pressure, such as across the capillary bed.
[latex]Q=\frac{P_1-P_2}{R}[/latex]
The myogenic response regulating blood flow within the kidney depends upon a characteristic shared by most smooth muscle cells of the body. When you stretch a smooth muscle cell, it contracts; when you stop, it relaxes. This mechanism works in the afferent arteriole that supplies the glomerulus. When blood pressure increases, smooth muscle cells in the wall of the arteriole are stretched and respond by contracting to increase resistance, resulting in little change in flow. When blood pressure drops, the same smooth muscle cells relax to lower resistance, allowing a continued even flow of blood. As you can see from the equation above, an increase in both pressure and R will result in Q remaining constant.
This mechanism of regulation is essential to maintaining homeostasis at the kidney as increasing flow and glomerular pressure would result in increased filtration causing the loss of fluids from the body. Thus, autoregulation and the myogenic response are essential to prevent the loss of fluids from everyday activities such as standing up or exercising.
Stretching of blood vessels due to increased blood volume causes the blood vessel to rapidly decrease in diameter; pushing against the increased volume within the vessel. This results in increased resistance to blood flow, thus keeping the GFR constant.
The following video provides a quick and helpful explanation of autoregulation and the myogenic response related to the kidney. It refers to a graph of blood pressure plotted against blood flow similar to the one seen in the course notes. Information after 2:07 minutes is beyond the scope of this course.
Testing Your Knowledge
Clinical Application:
What happens when there is an inability to properly control and regulate the kidney vasculature? One of the main causes of chronic kidney disease is high blood pressure. How does high blood pressure alter the kidney’s function? Hint: Think about the ability to deliver blood and oxygen to the glomerular capillaries.
For more information on high blood pressure and the kidneys, check out this video by the National Kidney Foundation.
Controlling the Radius of Arterioles
The radius of the vessels can be controlled by the nervous system, by the endocrine system and locally by the paracrine and autocrine systems.
Nervous control:
The direct sympathetic nervous system (SNS) innervation of the vasculature in the kidney causes constriction. The sympathetic nervous system has a greater effect on the vasoconstriction of the afferent arterioles than the efferent arterioles.
Paracrine and Autocrine control:
Nitric oxide (NO) acts as a potent vasodilator on the afferent and efferent arterioles equally. ET-1 acts as a vasoconstrictor of both the afferent and efferent arterioles equally. Additionally, ADO and ATP are both vasoconstrictors that act on the afferent arterioles.
Endocrine control:
Epinephrine is a vasoconstrictor of the afferent arterioles greater than the efferent arterioles and angiotensin II is a vasoconstrictor of the efferent arterioles greater than the afferent arterioles. In contrast, ADH-VP acts as a vasoconstrictor on the afferent arterioles greater than the efferent arterioles. ANP is unique because it acts as a vasodilator of the afferent arterioles and a vasoconstrictor of the efferent arterioles.
Anytime the radius of the afferent and efferent arterioles are affected separately there is a change in pressure in the glomerulus (PG) which can cause a change in filtration at the kidney.
The following table explains how vasoconstriction of the afferent or efferent arterioles affects pressure in the glomerulus (PG). It may be useful to refer to this diagram when solving problems related to blood flow in the kidney. [2]
Table 1: How vasoconstriction and vasodilation of the afferent and efferent arterioles affect the pressure in the glomerulus.
| Arterioles | Vasoconstriction | Vasodilation |
|---|---|---|
| Afferent > Efferent | Decreases pressure in the glomerulus | Increases pressure in the glomerulus |
| Efferent > Afferent | Increases pressure in the glomerulus | Decreases pressure in the glomerulus |
| Afferent = Efferent | No change in glomerular pressure | No change in glomerular pressure |
Test Your Knowledge
Thinking Beyond:
Why is it so beneficial that the kidney can filter waste out of the blood when someone consumes high amounts of alcohol? Explain what happens in the kidney to reduce the blood alcohol level. Hint: Think about when/where the wastes will move in and out of the kidney.
Key Takeaways
Consider the following concepts to help guide your studies:
- The difference between paracrine/autocrine, endocrine and nervous control.
- How vasodilation or vasoconstriction affect PG.
- The effects of epinephrine and Angiotensin II.
Sub-chapter Quiz
The questions below can be used to assess your knowledge within this chapter. There are five multiple-choice questions that you should attempt without referring to your notes. The questions will provide you with responses to your answers to guide your studying but should not be used as your only resource.
Media Attributions
- Kidney Blood Flow © Wikimedia Commons adapted by Brittany Emary is licensed under a CC BY (Attribution) license
- Vasculature Flow (Map-MCFP) (2) © Lisa Kazuhara is licensed under a CC0 (Creative Commons Zero) license
- CC BY: Attribution Licensed Content. Provided by OpenStax. Located at https://openstax.org/books/anatomy-and-physiology/pages/25-3-gross-anatomy-of-the-kidney ↵
- CC BY-NC: Attribution-NonCommercial Licensed Content. Provided by OpenStax. Located at https://www.commons.wikimedia.org/wiki/File:2612_Blood_Flow_in_the_Kidneys.jpg ↵
Dense network of capillaries and the site where kidney filtration begins.
A mechanism of auto-regulation where vascular smooth muscle can contract in response to increasing pressure.
System of glands that produce hormones to regulate and control bodily activities.
Prepares the body to respond to stress, such as a threat or injury. It is often referred to as the “fight-or-flight” response.

