Calcium and Phosphate Regulation
Now that you have a foundational understanding of the classes, characteristics, signalling methods, and regulation of hormones let’s apply this knowledge while examining the regulation of calcium and phosphate within the human body. Within the body calcium and phosphate are inversely related: as blood calcium levels rise, phosphate levels fall. This is because phosphate binds to calcium reducing the available free calcium within the bloodstream. As a result, the tight regulation of both these minerals is essential to maintain nerve communication, muscle function, and the formation and restoration of bones. The regulation of calcium and phosphate results from the interactions of three hormones: parathyroid hormone, calcitonin, and vitamin D. This section will examine the roles of these hormones at the level of the bone, kidneys, and intestines in situations of calcium/phosphate deprivation and loading.
Learning Outcomes
In this section you will learn…
- The roles and relationships between calcium and phosphate in the body.
- The actions of parathyroid hormone, vitamin D, and calcitonin.
- How these hormones are used to regulate calcium and phosphate levels in situations of homeostatic imbalance.
Calcium Homeostasis
Calcium is an essential mineral due to its pivotal roles in muscle and nerve function discussed in the Communication: Principles chapter. Although essential, calcium cannot be produced by any biological process. As a result, calcium can only enter the body through the diet. Once absorbed by the gut into the bloodstream, plasma calcium exists either free and biologically available (50%), bound to its carrier protein albumin (40%), or complexed as part of biocarbonate (10%). Outside of the bloodstream, the bones act as a storage site for excess plasma calcium. The body deposits calcium in the bones when blood levels get too high and they release calcium when blood levels drop too low. In order to maintain essential bodily functions, plasma calcium levels are tightly regulated. The body regulates calcium homeostasis with two pathways; one is signaled when blood calcium levels are reduced below the normal range and the other pathway is signaled when blood calcium levels are elevated above the normal range. The learning object below is a basic summary of the two calcium homeostatic pathways. At this point in the subchapter, use this learning object to appreciate that plasma calcium levels are highly regulated within a narrow range using negative feedback loops. Additionally, use this learning object to familiarize yourself with the pathways associated with situations of calcium deprivation and loading. Keep in mind that these pathways will be discussed in further detail later in this section.
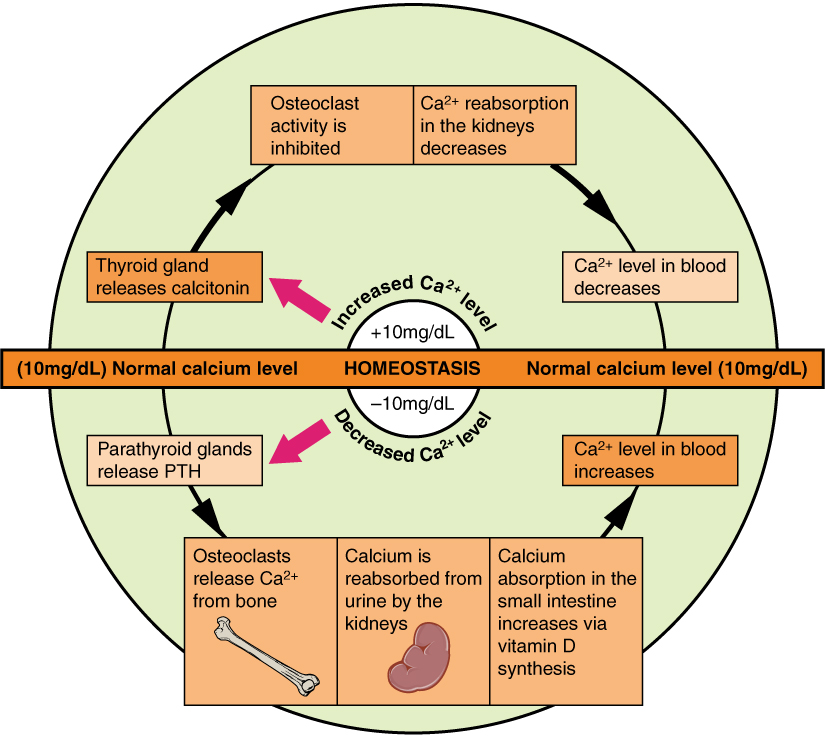
You may have noticed in the learning object above that there are three hormones that play an important role in regulating blood calcium homeostasis: [1] the parathyroid hormone (PTH), Vitamin D, and calcitonin. Before we discuss the homeostatic mechanisms behind calcium regulation, let us take a moment to introduce these hormones and consider their general characteristics.
Parathyroid Hormone
Parathyroid hormone (PTH) is a peptide hormone that is produced and released by chief cells of the parathyroid gland. Chief cells are specialized cells because they act as calcium sensors with corresponding receptors. Chief cells contain very specific calcium membrane receptors, that use calcium as the ligand. When calcium binds to these receptors a G-protein is activated which triggers a second messenger to alter PTH release. Through this mechanism, plasma calcium levels act as a regulator of PTH production and release. If plasma calcium levels are low chief cells will increase PTH release, and if plasma calcium are high chief cells will decrease PTH release. Chief cells are very sensitive, therefore only a small change in plasma calcium levels will result in a large change in PTH release.
Once PTH is released from chief cells of the parathyroid gland it circulates in the bloodstream mostly unbound. As mentioned previously, PTH is a peptide hormone. Think back to the previous section, what are some characteristics of peptide hormones? Peptide hormones are non-lipid soluble which means they are unable to cross the phospholipid bilayer and thus require receptors located on the plasma membrane to enter the cell. Additionally, peptide hormones, being NLS, can be stored in secretory vesicles of cells. This kind of hormonal storage is convenient because when chief cells are signalled to produce and release PTH, secretory cells can simply release stored PTH into the bloodstream to rapidly regulate blood calcium levels.
Vitamin D
Vitamin D is not classically considered a hormone but is required in order to produce the hormone calcitriol, 1,25-(OH)2-D3. Vitamin D can enter the bloodstream by either being absorbed by the gut from the diet or by sunlight interacting with 7-dehydrocholesterol within the skin. Once vitamin D is in the bloodstream, it travels to the liver where it binds to its corresponding receptor. Once inside the liver cells, an enzyme converts vitamin D into 25-OH-D. 25-OH-D then travels via the bloodstream to the kidneys where it binds to its corresponding receptor. Once inside the kidney cells, the enzyme 1-alpha-hydroxylase converts 25-OH-D into 1,25-(OH)2-D3 also known as calcitriol. Calcitriol is a steroid hormone that acts to regulate blood calcium levels. Think back to the previous section, what are some characteristics of steroid hormones? Steroid hormones are essentially all lipid-soluble which means they are able to cross the phospholipid bilayer to interact with their receptors located in the cytosol or nucleus of the cell. Additionally, steroid hormones, being LS, cannot be stored within secretory vesicles and can only be stored bound to their carrier portion or synthesized and secreted when needed.
Calcitonin
Calcitonin is a peptide hormone that is produced and released from parafollicular cells of the thyroid gland into the bloodstream. Peptide hormones are non-lipid soluble which means they are unable to cross the phospholipid bilayer and thus require receptors located on the plasma membrane to enter the cell. Additionally, calcitonin, being NLS, can be stored in secretory vesicles of cells. This kind of hormonal storage is convenient because when parafollicular cells are signaled to produce and release calcitonin, secretory cells can simply release stored calcitonin into the bloodstream to rapidly regulate blood calcium levels.
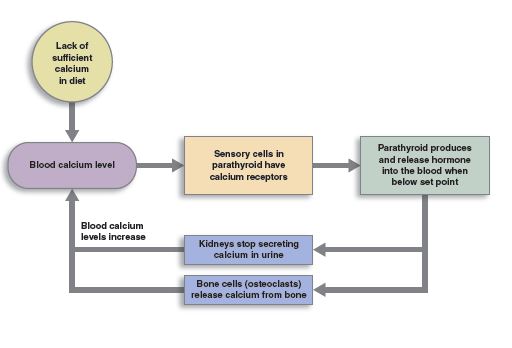
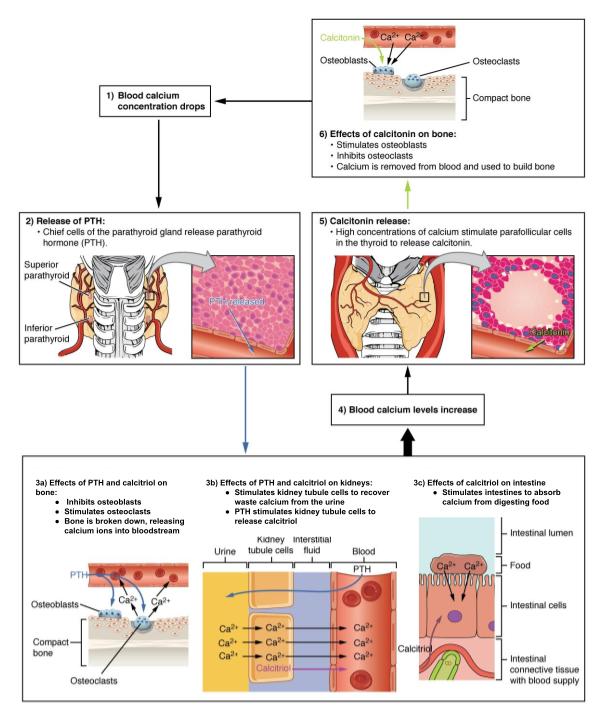
Decreased Blood Calcium Concentrations
A decrease in plasma calcium concentrations below the normal range is a condition called hypocalcemia. Since calcium is an essential mineral utilized for muscle contractions, hypocalcemia can cause impaired muscle function. As a result, it is imperative that the body acts to restore calcium homeostasis. As mentioned previously, chief cells of the parathyroid gland have plasma membrane receptors for calcium. When plasma calcium concentrations are low, calcium will not actively bind to their membrane receptors. This sends a signal to the chief cells of the parathyroid gland to increase the production and release of parathyroid hormone. PTH is released in hypocalcemic states in order to increase plasma calcium levels by targeting the bone and kidneys.[2]
In the bone, PTH binds to receptors to stimulate osteoclast activity. Osteoclasts secrete an enzyme responsible for bone reabsorption which is a process that breaks down bone tissue and releases minerals into the bloodstream. This bone demineralization process caused by osteoclast activity releases both calcium and phosphate from the bone into the bloodstream. As a result, PTH activity on the bones increases plasma calcium and phosphate concentrations. Additionally, PTH also inhibits osteoblast activity. Osteoblasts secrete an enzyme responsible for the formation of bone which utilizes minerals from the bloodstream. By inhibiting osteoblast activity it spares the utilization of calcium and phosphate thus preventing the decrease in their plasma concentrations.[3] In the kidneys, PTH binds to receptors to decrease the excretion of calcium from the urine while increasing the excretion of phosphate. As a result, PTH activity on the kidneys increases plasma calcium concentrations and decreases plasma phosphate concentrations. The learning object below is a basic summary of PTH’s actions at the bone and kidneys to regulate calcium homeostasis in response to decreased plasma concentrations.
Tips From Past Students
Here is a tip to help you differentiate between the roles of osteoblasts and osteoclasts:
OsteoBlasts Build Bone, whereas, OsteoClasts Consume Bone
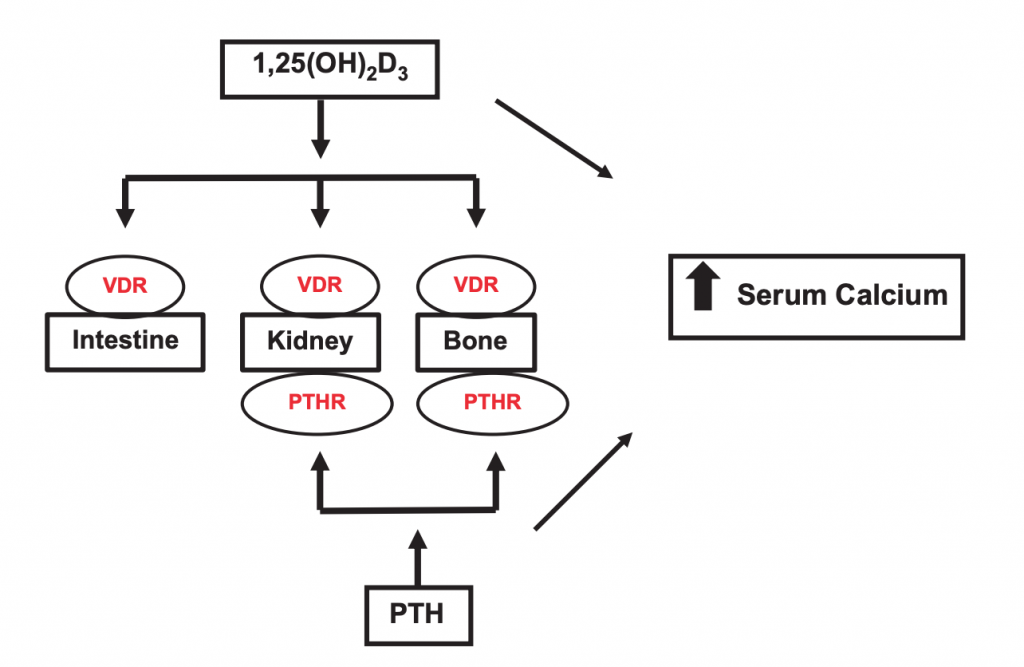
Finally, PTH activates the enzyme 1-alpha-hydroxylase in the kidney which converts 25-OH-D into calcitriol, the active form of vitamin D. The PTH-activated calcitriol also acts to increase plasma calcium levels by targeting the bone, kidneys, and intestines. In the bone, calcitriol stimulates osteoclast activity and inhibits osteoblast activity which increases plasma calcium and phosphate concentrations. In the kidneys, calcitriol decreases the excretion of calcium from the urine which increases plasma calcium concentrations. Lastly, in the intestines, calcitriol binds to receptors to increase the absorption of calcium and phosphate from the diet which increases plasma calcium and phosphate concentrations.[4] Although not necessary at this point in the course, further details about the mechanisms behind calcium and phosphate absorption can be found in the Digestion and Absorption subchapter.
At this point, the effects of the hormones at different locations throughout the body may seem abstract. If this is the case, examine the learning object below to help you visualize PTH and calcitriol’s actions on different structures throughout the body. The key takeaway from this learning object is that PTH acts directly on the bone and kidneys while calcitriol acts on the bone, kidneys, and intestines to increase plasma calcium concentrations. Although specified in this learning object, you are not required to know the corresponding hormone receptors labeled in red text.
Once these processes act to increase plasma calcium concentrations back within the normal range there will be enough calcium to actively bind to plasma membrane receptors on the surface of chief cells. The binding of calcium to the plasma membrane receptors will send a negative feedback signal to decrease the production and release of PTH.[5]
Now that you understand how the body acts to regulate calcium in response to a decrease in plasma calcium concentrations consider how it would act in response to an increase in concentrations above the normal range. Before reading any further take this opportunity to anticipate how the body would respond to an increase in plasma calcium concentrations by working through the above mechanisms in reverse. You can check your response by reading the following section.
Test Your Knowledge
Clinical Application:
While getting a blood test, a doctor notices that you have high PTH levels. What other levels might they find are either higher or lower than normal and why? What are some of the implications of these results? Hint: Consider in what state there is an increase in PTH production/release and what other hormones act to maintain homeostasis.
Increased Blood Calcium Concentrations
An increase in plasma calcium concentrations above the normal range is a condition called hypercalcemia. Hypercalcemia can cause weakness of bones due to high osteoclast activity. As a result, it is imperative that the body acts to restore calcium homeostasis. As mentioned previously, chief cells of the parathyroid gland have plasma membrane receptors for calcium. When plasma calcium concentrations are high a signal is sent to the chief cells of the parathyroid gland to decrease the production and release of parathyroid hormone. PTH is inhibited in hypercalcemic states in order to decrease plasma calcium levels by targeting the bone and kidneys.[6]
In the bone, the inhibition of PTH will stimulate osteoblast activity. Osteoblasts secrete an enzyme responsible for the formation of bone which utilizes minerals from the bloodstream. This process utilizes calcium and phosphate which will act to decrease their plasma concentrations. Additionally, PTH also inhibits osteoclast activity. Osteoclasts secrete an enzyme responsible for bone reabsorption which is a process that breaks down bone tissue and releases minerals into the bloodstream. By inhibiting osteoclast activity it prevents the release of calcium and phosphate from the bone into the bloodstream. As a result, the inhibition of PTH activity on the bones decreases plasma calcium and phosphate concentrations.[7] In the kidneys, the inhibition of PTH increases the excretion of calcium from the urine while decreasing the excretion of phosphate. As a result, the inhibition of PTH activity on the kidneys decreases plasma calcium concentrations and increases plasma phosphate concentrations.
Finally, the inhibition of PTH prevents the activation of the enzyme 1-alpha-hydroxylase in the kidney. As you may recall 1-alpha-hydroxylase acts convert 25-OH-D into calcitriol, the active form of vitamin D. The inhibition of PTH preventing the formation of calcitriol will act to decrease plasma calcium levels by targeting the bone, kidneys, and intestines. In the bone, the lack of calcitriol will stimulate osteoblast activity and inhibit osteoclast activity which decreases plasma calcium and phosphate concentrations. In the kidneys, the lack of calcitriol increases the excretion of calcium from the urine which decreases plasma calcium concentrations. Lastly, in the intestines, the lack of calcitriol decreases the absorption of calcium and phosphate from the diet which decreases plasma calcium and phosphate concentrations.[8]
Once these processes act to decrease plasma calcium concentrations back within the normal range there will be sufficient calcium levels to actively bind to plasma membrane receptors on the surface of chief cells. The binding of calcium to the plasma membrane receptors will send a negative feedback signal to stop the inhibition of the production and release of PTH.[9]
Another hormone that we have not yet discussed in the context of calcium regulation is calcitonin. When blood calcium concentrations are high the parafollicular cells of the thyroid gland stimulate the release of calcitonin. Calcitonin is also released in hypercalcemic states in order to decrease blood calcium levels by targeting the bone. In the bone, calcitonin binds to receptors to stimulate osteoblast activity and inhibit osteoclast activity which decreases plasma calcium and phosphate concentrations. Once this process act to decrease plasma calcium concentrations back within the normal range a negative feedback signal will be sent to the parafollicular cells of the thyroid gland to decrease the production and release of calcitonin.[10]
Test Your Knowledge
Clinical Application:
A tumor is found on 1 of the 4 parathyroid glands in your body. This tumor is acting to prevent the release of PTH in the body. What other effects will this have on the body and why? Hint: Consider the roles of parathyroid hormone in calcium/phosphate regulation.
Before reading any further make sure you have a concrete understanding of the different hormones utilized during calcium regulation and their corresponding effects. This knowledge will be required to fully understand phosphate homeostasis in the following section. If you are having trouble visualizing the calcium homeostatic pathways examine the learning object below. This flow chart does an excellent job summarizing the hormones and their corresponding effects in both hypercalcemic and hypocalcemic states. While examining this learning object keep in mind that it only depicts the calcitonin response to an increase in blood calcium levels. Although not depicted, recall that in response to an increase in blood calcium concentration PTH production and release is also inhibited which acts to reverse its typical effects. You may want to take this opportunity to talk yourself through how exactly the inhibition of PTH reduces blood calcium concentrations at the bone, kidneys, and intestines.
Tips From Past Students
The following is a summary of key points to help you understand the mechanisms of action behind each hormone,
- PTH increases plasma calcium levels by acting on the bone and kidneys.
- Vitamin D increases plasma calcium levels by acting on the bone, kidneys, and intestines.
- Calcitonin decreases plasma calcium levels by acting on the bone.
Phosphate Homeostasis
As mentioned previously within the body calcium and phosphate are inversely related: as blood calcium levels rise, phosphate levels fall. This is because phosphate binds to calcium reducing the available free calcium within the bloodstream. As a result of this relationship, it is imperative that both levels of calcium and phosphate are tightly regulated. Even though mentioned above calcium regulation affects local phosphate levels at the bone, kidney, and intestines it is important to note that there is no net effect on plasma phosphate levels. However, let’s consider homeostatic mechanisms in situations of phosphate deprivation and loading.
Increased Blood Phosphate Concentrations
An increase in plasma phosphate concentrations above the normal range is a condition called hyperphosphatemia. In a hyperphosphatemic state, the excess phosphate will bind to calcium decreasing its plasma concentrations causing the overproduction of PTH. If PTH is overproduced, this results in hyperparathyroidism which can lead to excessive amounts of calcium being released into the blood. As a result, it is imperative that the body acts to restore phosphate homeostasis. An increase in plasma phosphate concentrations inhibits the production of calcitriol, the active form of vitamin D. Before reading any further take a moment to consider the ramifications of the inhibition of calcitriol production. As you may have recalled the inhibition of calcitriol production will act to decrease plasma phosphate levels by targeting the bone, kidneys, and intestines. In the bone, the lack of calcitriol will stimulate osteoblast activity and inhibit osteoclast activity which decreases plasma calcium and phosphate concentrations. In the intestines, the lack of calcitriol decreases the absorption of calcium and phosphate from the diet which decreases plasma calcium and phosphate concentrations. Lastly, in the kidneys, the lack of calcitriol increases the excretion of calcium from the urine which decreases plasma calcium concentrations.[11] All of these mechanisms act to decrease plasma phosphate levels which will send a negative feedback signal to no longer inhibit calcitriol production. You may have noticed that even though all of these mechanisms act to decrease plasma phosphate levels they also act to cause a net decrease in plasma calcium concentrations. As a result, the body must now act to fix the calcium imbalance. Take this opportunity to test yourself on how the body responds to a decrease in plasma calcium concentrations.
Decreased Blood Phosphate Concentrations
A decrease in plasma phosphate concentrations below the normal range is a condition called hypophosphatemia. In a hypophosphatemic state, the reduction in plasma phosphate levels causes an increase in plasma calcium concentrations causing the underproduction of PTH. If PTH is underproduced, this results in hypoparathyroidism which can lead to very low levels of calcium in the blood. As a result, it is imperative that the body acts to restore phosphate homeostasis. A decrease in plasma phosphate concentrations stimulates the production of calcitriol, the active form of vitamin D. Before reading any further take a moment to consider the ramifications of an increase in calcitriol. As you may have recalled calcitriol acts to increase plasma calcium levels by targeting the bone, kidneys, and intestines. In the bone, calcitriol stimulates osteoclast activity and inhibits osteoblast activity which increases plasma calcium and phosphate concentrations. In the intestines, calcitriol binds to receptors to increase the absorption of calcium and phosphate from the diet which also increases plasma calcium and phosphate concentrations. Lastly, in the kidneys, calcitriol decreases the excretion of calcium from the urine which increases plasma calcium concentrations.[12] All of these mechanisms act to increase plasma phosphate levels which will send a negative feedback signal to no longer stimulate the production of calcitriol. You may have noticed that even though all of these mechanisms act to increase plasma phosphate levels they also act to cause a net increase in plasma calcium concentrations. As a result, the body must now act to fix the calcium imbalance. Take this opportunity to test yourself on how the body responds to an increase in plasma calcium concentrations.
Test Your Knowledge
Real Life Scenario:
Chronic kidney disease can be found to significantly decrease the activity of 1-alpha hydroxylase. Would this disease be more closely associated with hyperparathyroidism or hypoparathyroidism and why? Hint: Consider the actions and ramifications of 1-alpha hydroxylase.
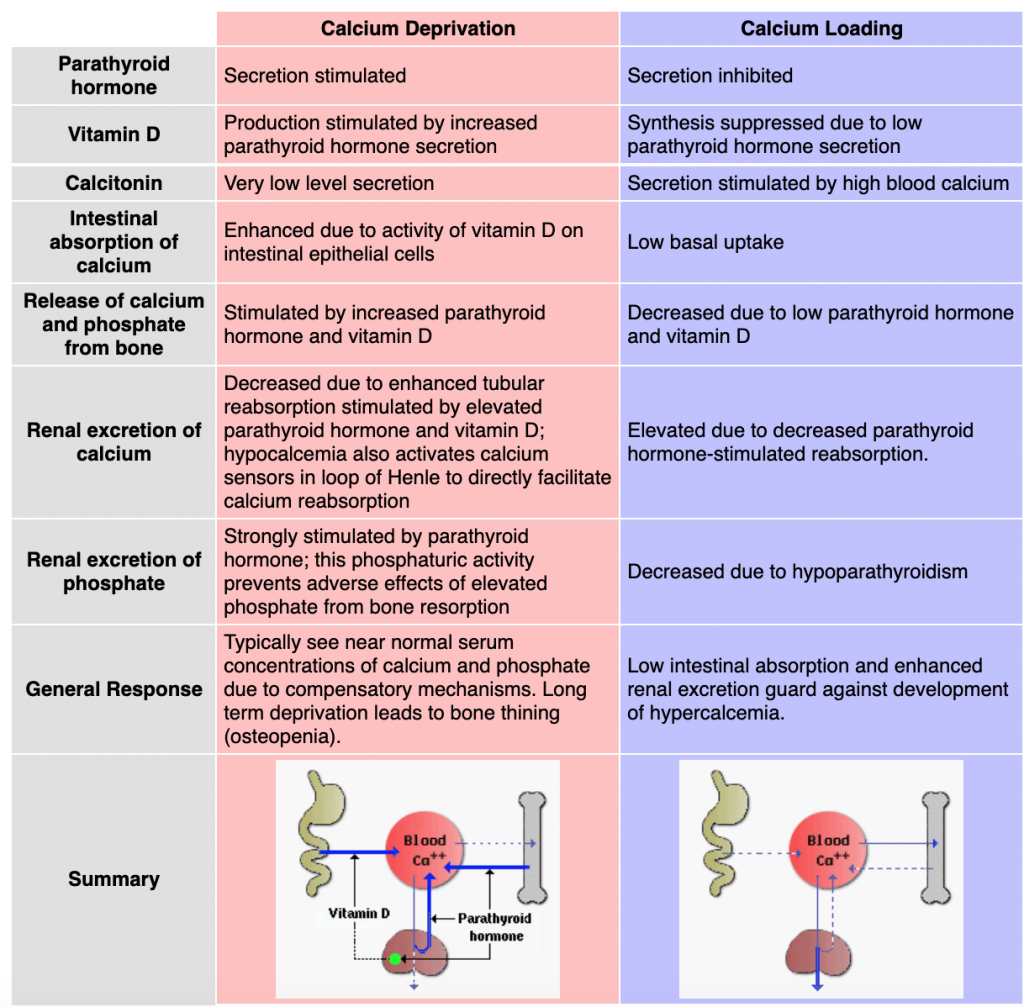
Overview of Calcium/Phosphate Homeostasis
Now that we have discussed in detail the hormonal regulation of calcium and phosphate levels within the body let’s take a step back and review some of the key points. The learning object below is a helpful study tool that summarizes the actions and corresponding effects of PTH, vitamin D, and calcitonin in response to situations of calcium deprivation and loading in order to restore calcium homeostasis. Also, take a moment to consider this learning object in the context of phosphate homeostasis. Although not specified in this learning object, recall that the homeostatic response to increased blood phosphate levels leads to a calcium deprivation problem and the homeostatic response to decreased blood phosphate levels leads to a calcium loading problem.
Lastly, to wrap up our discussion on calcium and phosphate homeostasis the following video does an excellent job recapping the key points discussed throughout this subchapter. Keep in mind that this video simply acts as a summary to supplement your learning and should act as the sole focus of your study. Although I would highly recommend watching the following video in its entirety, here is a list of the key topics with the corresponding timings: calcium physiological functions (0:00 – 1:23), hormone introductions (1:23 – 2:12), hormone actions (2:12 – 3:44), hypercalcemia (3:44 – 4:31), hypocalcemia (4:31 – 5:06).
“Calcium Homeostasis: Regulation & Maintenance” by AMBOSS Medical Knowledge Distilled is All Rights Reserved.
Tips From Past Students
Now that we have reached the end of this subchapter you may be feeling overwhelmed with the amount of hormones and mechanisms involved in calcium homeostasis when in fact it is much simpler than it may originally appear. We found the best way to tackle studying this subchapter is to first understand the actions of each hormone. Once you understand the actions you can logically apply the hormones, either by stimulating or inhibiting, in order to address a calcium or phosphate imbalance. Try talking yourself through or drawing a flow chart to address how the body responds to states of hypercalcemia/hypocalcemia and hyperphosphatemia/hypophosphatemia.
Key Takeaways
Consider the following concepts to help guide your studies:
- At what location(s) in the body each hormone acts on.
- How the body regulates plasma calcium concentrations in response to hypocalcemia and hypercalcemia.
- How the body regulates plasma phosphate concentrations in response to hypophosphatemia and hyperphosphatemia.
- The ramifications if one of the hormones involved in calcium/phosphate homeostasis were under or overproduced.
Subchapter Quiz
The questions below can be used to assess your knowledge within this chapter. There are five multiple-choice questions that you should attempt without referring to your notes. The questions will provide you with responses to your answers to guide your studying but should not be used as your only resource.
Media Attributions
- Pathways in Calcium Homeostasis © OpenStax CNX is licensed under a CC BY (Attribution) license
- PTH control of blood calcium © Open Learning Initiative is licensed under a CC BY (Attribution) license
- Low Serum Calcium © Vaishali Veldurthy is licensed under a Public Domain license
- PTH Actions in Calcium Homeostasis © OpenStax CNX adapted by Krista Pearce is licensed under a CC BY (Attribution) license
- Private: Summary: Calcium Deprivation/Loading © Richard Bowen is licensed under a CC BY-SA (Attribution ShareAlike) license
- Betts, G. J., Young, K. A., Wise, J. A., Johnson, W., Poe, B., Kruse, DH., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2013). Calcium Homeostasis. Anatomy and Physiology. ↵
- Lumen (n.d.). Regulation of Body Processes. Biology for Majors II. ↵
- Lumen (n.d.). Regulation of Body Processes. Biology for Majors II. ↵
- Betts, G. J., Young, K. A., Wise, J. A., Johnson, W., Poe, B., Kruse, DH., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2013). Calcium Homeostasis. Anatomy and Physiology. ↵
- Betts, G. J., Young, K. A., Wise, J. A., Johnson, W., Poe, B., Kruse, DH., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2013). Calcium Homeostasis. Anatomy and Physiology. ↵
- Lumen (n.d.). Regulation of Body Processes. Biology for Majors II. ↵
- Lumen (n.d.). Regulation of Body Processes. Biology for Majors II. ↵
- Betts, G. J., Young, K. A., Wise, J. A., Johnson, W., Poe, B., Kruse, DH., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2013). Calcium Homeostasis. Anatomy and Physiology. ↵
- Betts, G. J., Young, K. A., Wise, J. A., Johnson, W., Poe, B., Kruse, DH., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2013). Calcium Homeostasis. Anatomy and Physiology. ↵
- Betts, G. J., Young, K. A., Wise, J. A., Johnson, W., Poe, B., Kruse, DH., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2013). Calcium Homeostasis. Anatomy and Physiology. ↵
- Betts, G. J., Young, K. A., Wise, J. A., Johnson, W., Poe, B., Kruse, DH., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2013). Calcium Homeostasis. Anatomy and Physiology. ↵
- Betts, G. J., Young, K. A., Wise, J. A., Johnson, W., Poe, B., Kruse, DH., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2013). Calcium Homeostasis. Anatomy and Physiology. ↵
A hormone secreted by the parathyroid glands that plays a role in regulating blood calcium concentration.
A nutrient in food that is converted into an active hormone that aids in controlling plasma calcium concentration.
A hormone produced by the parafollicular cells of the thyroid gland. Aids in the regulation of plasma calcium levels.
A condition characterized by blood calcium levels that are lower than normal.
Cells responsible for reabsorbing (breaking down) bone.
Cells responsible for forming new bone.
A condition characterized by blood calcium levels that are higher than normal.
A condition characterized by blood phosphate levels that are higher than normal.
A condition in which the parathyroid gland is producing and releasing too much parathyroid hormone, resulting in an increase in blood calcium levels.
A condition characterized by blood phosphate levels that are lower than normal.
A condition in which the parathyroid gland is producing and releasing too little parathyroid hormone, resulting in low levels of blood calcium.

