Fluid Flux & The Lymphatic System
You may be wondering why we're bothering to cover fluid flux and the lymphatic system in the cardiovascular chapter... at first glance, the two seem very unrelated. However, it all comes back to the control of blood pressure. Without the ability to filter fluid out of the capillaries and into the lymphatic system, individuals would experience swelling. This build-up of fluid would cause heightened blood pressure edema, and other very serious medical conditions. As you read through this section, make sure you can appreciate how the cardiovascular and lymphatic systems rely on each other and how they affect the body.
Learning Outcomes
In this section you will learn...
- The difference between filtration and reabsorption using terms like oncotic pressure and hydrostatic pressure.
- To properly apply Starling's Equation.
- How the cardiovascular and lymphatic systems are interconnected and reliant on one and other.
Capillary Exchange
Interstitial Fluid
What comes to mind when I ask you to think about fluid in the human body? Your first thought is likely going to be about blood. Of course, blood is a bodily fluid that performs a great many functions to keep us alive. However, blood is not the most abundant fluid in the body. A healthy human body contains 5 litres of blood, but has 11 litres of interstitial fluid. Before we begin discussing fluid flux, let's break down interstitial fluid.
Interstitial fluid is a gel-like solution that surrounds cells in the body. This fluid is mainly composed of water but contains a great many substances. Due to this, the interstitial fluid acts as a passage for capillaries and tissues. O2 (oxygen) can travel from the capillary into the interstitial fluid and to the tissue. CO2 (carbon dioxide) can move from the tissue through the interstitial fluid and back into the capillary. The interstitial fluid keeps our cells alive, and in turn, keeps us alive!
The video below is a great introduction to the unit and will go into greater detail about interstitial fluid. Given that the video is less than 5 minutes long, I'd recommend watching the whole thing in order to preface the rest of this chapter. Keep in mind that the interstitial fluid is in the interstitial space (ISS). Many individuals will refer to these terms interchangeably so don't worry if you hear both terms.
Capillaries
Let’s shift from the interstitial fluid to the capillaries. Capillaries are the smallest form of blood vessels and help transfer nutrients and O2 throughout the system. There are three ways that nutrients are pushed out of the capillaries and into the tissues. In this course, we will mainly focus on bulk flow. Bulk flow is the movement of solutions across the capillary wall to get from a high-pressure area to a low-pressure area. While this may sound similar to diffusion, there is a slight difference. Diffusion is a slower motion, whereas bulk flow moves all at once (hence the name bulk). Bulk flow is dependent on hydrostatic pressure and oncotic pressure from the capillaries, so let’s go over these terms below.
Hydrostatic pressure is the force that pushes fluid out of the capillary and into the interstitial space. This pressure contributes to filtration out of the capillary. Hydrostatic pressure is created by the heart and is heavily influenced by blood pressure. High blood pressure will lead to increased hydrostatic pressure, and therefore, greater fluid content being pushed out of the capillary and into the interstitial space. It is important to note that hydrostatic pressure is not consistent throughout the capillary. As blood travels through the capillary, it interacts with the vessel wall and loses speed. The decrease in speed results in reduced blood pressure further down the capillary. While no difference is seen at first, hydrostatic pressure will be reduced later in the capillary, leading to decreased filtration.
On the other hand, oncotic pressure is the force that pulls fluid back into the capillary. This pressure is created by plasma proteins and will help contribute to reabsorption back into the capillary. Unlike hydrostatic pressure, oncotic pressure is consistent throughout the capillary as it is not reliant on blood pressure.
The video below is a useful resource as it describes these terms and uses visual aids. It is also a helpful refresher on blood vessels, specifically endothelial cells, during the first 2 minutes. All three ways to move nutrients to the tissues will be discussed, and the video will introduce the concept of filtration versus reabsorption through osmotic pressure at the 6:30 minute mark.
The terms oncotic pressure and colloid osmotic pressure can be used interchangeably. Both terms are simply describing a type of osmosis, the reabsorption of fluid from the interstitial space back into the capillaries... so don't worry about getting them mixed up. It's not as complex as it sounds.
Oncotic Vs. Hydrostatic Pressure
It is important to recognize there are two hydrostatic pressures; one from the capillary and one from the interstitial fluid. As mentioned previously, the hydrostatic pressure in the capillary varies according to changes in blood pressure. However, in the interstitial fluid, this pressure will not change. The hydrostatic pressure from the interstitial space is maintained around 0 via lymphatic vessels. These vessels work to carry away extra fluid and therefore help control hydrostatic pressure. Don’t worry too much about these vessels right now, as they will be explained in greater detail later in this section. Similarly, there are two oncotic pressures; one from the capillary and one from the interstitial fluid. The interstitial fluid oncotic pressure is also small and will have little effect on bulk flow.
The video below describes these concepts in greater detail and uses helpful analogies. Interstitial fluid pressure is discussed and its impact on the pressure gradient in the capillary is explained.
Test Your Knowledge
Thinking Beyond:
Complete the table below to strengthen your understanding of hydrostatic pressure and oncotic pressure. Hint: Remember that oncotic pressure causes fluid to flow into the capillary, and hydrostatic pressure causes fluid to flow out.
| Pressure | Hydrostatic | Oncotic |
|---|---|---|
| Direction of fluid?
|
||
| How is the pressure generated?
|
||
| Where in the capillary is the pressure greatest?
|
||
| Does the pressure promote filtration or reabsorption?
|
Fluid Flux
Tissue Fluid Formation
Let’s combine the concepts discussed above to understand fluid flux. At the arterial end of the artery, hydrostatic pressure is greater than oncotic pressure. As a result, nutrients will be filtered out of the capillary and into the interstitial fluid. Here, the nutrients will travel to the tissues and provide them with a source of nourishment. At the venous end of the capillary, oncotic pressure is more significant than hydrostatic pressure. Fluid from the interstitial space will be reabsorbed into the capillary. Reabsorbed alongside this fluid are unwanted substances from the tissues, such as CO2. These substances will travel into the veins, where they will return to the heart to be oxygenated, and the cycle repeats.
The video below is useful as it applies a much more mathematical approach to filtration and reabsorption properties, whereas the last few have been very visual. At 3:15, the video explains how we can use the mathematical approach to determine which direction fluid is moving at a given time.
Test Your Knowledge
Clinical Application:
Unfortunately, you have discovered a blood clot has formed on the venular side of one of your capillaries. Using your knowledge of fluid flux, explain what would happen to your net fluid movement. Hint: Remember that hydrostatic pressure changes according to location in the capillary.
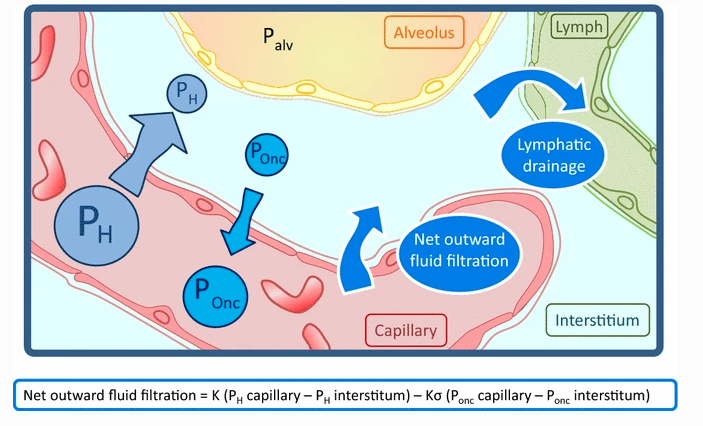
Fluid Flux Summary Diagram
This image was included because it clarifies all the components we've discussed thus far and highlights that the hydrostatic pressure out is realistically depicted as greater than the oncotic pressure into the capillary. The diagram introduces the drainage of fluid into the lymphatic system in addition to alveolar (pressure in the lungs), which is covered in another chapter.
Starling's Equation
Starling's Equation is a formula used to determine the net flow of fluid between capillaries and interstitial space. It is the mathematical equivalent to the fluid flux summary diagram included above.
Although the equation may look intimidating, all it is asking is...
- What is the difference in hydrostatic pressure in the capillary and in the interstitial space:
[latex](P_c − P_i)[/latex]
- What is the difference in oncotic pressure in the capillary and in the interstitial space:
[latex](π_c − π_i)[/latex]
Having this information can help determine which direction fluid is moving and whether filtration or reabsorption is the dominant force. Please find the equation below.
[latex]J_v = K [(P_c − P_i) − σ (π_c − π_i)][/latex]
Factors of Starling's Equation
Lets break down the different factors of [latex]J_v = K [(P_c − P_i) − σ (π_c − π_i)][/latex] :
K (or CFC): The capillary filtration rate. How permeable the capillaries are. This does not generally change so don't focus too hard on this variable.
PC (capillary pressure): Hydrostatic pressure exerted by the capillary content on capillaries.
Pt (hydrostatic pressure of interstitial space): Hydrostatic pressure exerted by surrounding tissue on the capillary. Can be negative, meaning it pulls fluid into the ISS.
πC (colloid osmotic pressure in capillaries): Fluid movement by osmosis (water moves from low protein concentration to high protein concentration) from ISS into capillaries.
πt (colloid osmotic pressure in the tissue): Osmotic pressure to move fluid from capillaries to ISS.
Additionally, the difference in hydrostatic pressure can be abbreviated to [latex]ΔP = (P_c − P_t)[/latex]. The difference in colloid osmotic pressure can be abbreviated to [latex]Δπ = (π_c − π_t)[/latex].
Applying JFluid
In any scenario we must consider how the these factors are affected by bodily function or how dis-regulators can affect these variables. Consider how the following scenarios would affect the above variables:
- Hyperproteinemia - excess protein in the blood
- High blood pressure
- Heart failure
- Edema - excess fluid in the tissue
How would this affect JFluid? Keep in mind that often situations will affect only affect one of [latex]ΔP = (P_c − P_t)[/latex] or [latex]Δπ = (π_c − π_t)[/latex].
ΔP: Overall fluid movement from capillaries to ISS.
Δπ: Overall fluid movement from ISS to capillaries.
When ΔP > Δπ the body is filtering out of capillaries.
When ΔP < Δπ the body is reabsorbing back into the capillaries.
Test Your Knowledge
Thinking Beyond:
Name a situation where multiple fluid flux variables would be manipulated at the same time. Hint: Think about what would happen to your body if you were dehydrated...
Visualizing ΔP and Δπ
This image was included because it depicts ΔP and Δπ in a healthy individual and is a useful graph that is necessary to know for examinations.
Keep in mind that [latex]HP_c = ΔP[/latex] and [latex]COP_r = Δπ[/latex].
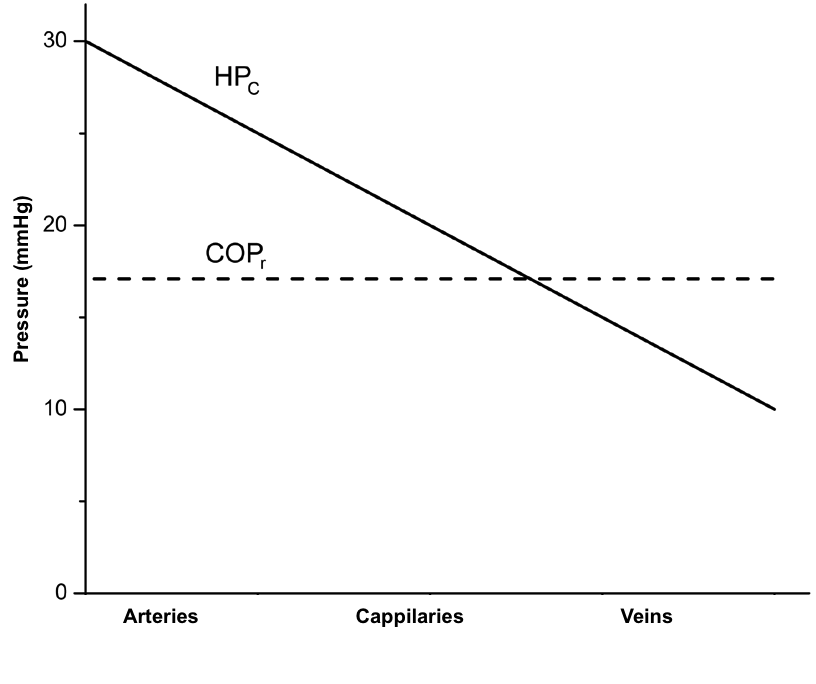
The slope of these lines will usually stay the same in our examples. Try and predict how the graph will change in each of the above practice scenarios (i.e. will ΔP or Δπ be higher or lower?). Additionally, look at the difference in the ratio of Filtration vs. Reabsorption in the scenarios compared to baseline.
Test Your Knowledge
Real-Life Scenario:
After falling asleep in class, you get locked in ROZH 101 over reading week! You have sufficient water but no food. As your body enters starvation, you suffer from low protein content (including plasma protein concentration). What effect will this have on oncotic pressure How will this change in oncotic pressure affect filtration and reabsorption in the body? Hint: Think about how dehydration would impact blood volume and plasma protein concentration.
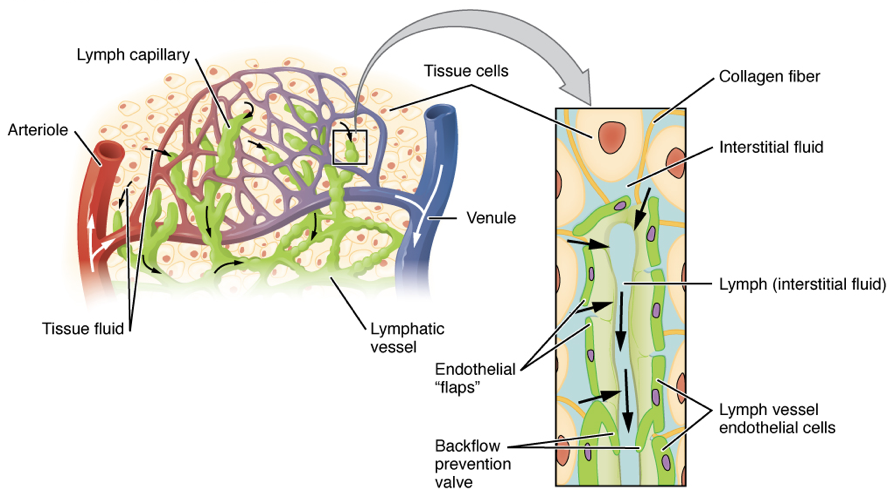
The Lymphatic System
As we have learned, more fluid is filtered out in a healthy human than is reabsorbed back into the capillaries. So what happens to this fluid? It is taken up by the lymphatic system. The filtered fluid is pushed out into the interstitial space, where it eventually enters the lymph vessels. These vessels are areas of low pressure, therefore, the fluid is drawn towards them. Once in the vessel, the fluid is contained due to one-way valves preventing back-flow. Skeletal muscle works alongside the lymphatic system to push the fluid from these vessels to two lymphatic ducts in the neck. Here, the fluid re-enters the cardiovascular system, and the process is repeated.
You may be wondering why the body goes through this whole process rather than leaving the fluid in the interstitial space. This is to prevent swelling. Abnormally large amounts of fluid in the interstitial space will cause the body to swell. The expansion present with swelling increases blood pressure and can cause edema. Edema can interfere with blood vessels and interrupt circulation, causing serious repercussions. Therefore, our lymphatic system must work alongside the cardiovascular system to maintain homeostasis.
Lymphatic System Diagram
The diagram below is helpful to understand how the lymphatic system is interlaced within the cardiovascular system. It highlights how the lymphatic capillaries are anchored by collagen fibers in the tissue. We can also see the lymphatic vessels that are responsible for taking up filtered fluid to prevent swelling. The close-up diagram displays the direction of fluid flow and shows the valves that will prevent backflow.
Lymphatic System Video
The video below covers the lymphatic system to the extent you need to know for this chapter. It also provides several real-world situations and their impact on the system. These scenarios help substantiate how important this system is and provides an excellent context for the exam questions.
Key Takeaways
Consider the following concepts to help guide your studies:
- Oncotic pressure forces fluid into the capillary from the ISS.
- Hydrostatic pressure forces fluid from the capillary into the ISS.
- We can use Starling’s Equation to determine the direction of fluid.
- The relationship between the cardiovascular system and lymphatic system is important as it influences blood pressure.
- Maintaining blood pressure is necessary to ensure that serious medical issues, such as edema, do not occur.
Subchapter Quiz
The questions below can be used to assess your knowledge within this chapter. There are five multiple-choice questions that you should attempt without referring to your notes. The questions will provide you with responses to your answers to guide your studying but should not be used as your only resource.
Media Attributions
- Physiology of Lung Water © Mathieu Jozwiak, Jean-Louis Teboul & Xavier Monnet is licensed under a CC BY (Attribution) license
- Schematic-presentation-of-the-Starling-oncotic-hypothesis-of-capillaries-HP-c-1 © Marijan Klarica is licensed under a CC BY (Attribution) license
- Lymph capillaries in the tissue spaces © J. Gordon Betts, Kelly A. Young, James A. Wise, Eddie Johnson, Brandon Poe, Dean H. Kruse, Oksana Korol, Jody E. Johnson, Mark Womble, Peter DeSaix is licensed under a CC BY (Attribution) license
Swelling caused by tissue leakage.
Extracellular fluid found throughout the whole body.
A protein which provides structural support to connective tissues, muscles, and skin.

