Control and Regulation of Blood Gases
Now that you know how we breathe, we must also learn how to control these mechanisms. This section will look at how we manage our breathing, both voluntarily and involuntarily, through neural control. We will dive deeper into the coordinating centre located in the brain and the concept of override. It also looks at the role of effectors, chemoreceptors, stretch receptors, high-pressure baroreceptors, and irritant receptors.
Learning Outcomes
In this section you will learn…
- How to describe the integration at the coordinating centre as it relates to voluntary and involuntary breathing.
- How to explain the neural pathway that controls breathing and the negative feedback that exists within the pathway.
- How to describe the unique roles of chemoreceptors, stretch receptors, high-pressure baroreceptors, and irritant receptors in the regulation of breathing.
The following learning object is a good overview of this subchapter and may be good to watch once you have become comfortable with the content and serve as a review. Between 3:46-7:48 minutes you will find the most relevant information to physiology as they discuss the anatomy of the thorax, nervous control over the effectors (2:11), override by the cerebral cortex (3:46), chemoreceptors (peripheral 4:50 and central 5:50), and other important receptors (6:20). The information presented within the first 2:10 is above course level as it goes into detail about the varying regions of the brain stem important for respiration. Key takeaways from the video include that higher brain centers allow for the voluntary control of breathing and change the rate of ventilation. It is also important to know the functions of all receptors mentioned, i.e., chemoreceptors, muscle, irritant, and stretch receptors.
Integration at the Coordinating Centres
As you’ve seen on a few occasions now, breathing is regulated by various coordinating centres in the brain and their integration of information is critical in respiration. We’ll take a little deeper dive into the types of centres and how the regulate different types of respiration.
Involuntary Respiration
Involuntary respiration is any form of respiration that occurs without conscious control. Involuntary respiration is controlled by the coordinating centre, or the brainstem, which is responsible for controlling the body’s many involuntary and metabolic functions.
The coordinating centre contains chemoreceptors, that monitor pH levels in the blood. These receptors send signals to the coordinating centre to adjust the ventilation rate to control acidity by increasing or decreasing the removal of carbon dioxide. We will be discussing chemoreceptors in greater detail later on in this chapter.
The coordinating centre then sends nervous impulses to the effectors, which are the diaphragm and the external intercostal muscles in this case. The nervous impulses lead to these skeletal muscles’ contraction, which increases the breathing rate and the volume of the lungs during inspiration.
Test Your Knowledge
Clinical Application:
Certain injuries can affect the nerves involved in breathing. A cervical spinal cord injury affects the spinal nerves that control the body’s respiratory muscles. A complete spinal cord injury affecting the cervical spinal cord will impact the diaphragm as well as the intercostal and abdominal muscles and limit a patient’s ability to breathe. How would this decrease in breathing capability impact the PaCO2 and PaO2 in a patient’s blood? How might the body try to compensate for these changes in blood gases? Hint: Think about how this decrease in ventilation will impact flow.
Voluntary Respiration
Voluntary respiration is any form of respiration that is under conscious control. This is important for higher functions that involve breathing, such as blowing out candles, talking, or holding our breath. Voluntary respiration is controlled by the cerebral cortex, which is responsible for controlling the body’s higher-order functions. Aspects of voluntary respiration may override involuntary respiration. For example, when we are talking, the cerebral cortex overrides the coordinating centre to inhibit our regular breathing pattern. This is why we can’t breathe in and speak at the same time.
However, voluntary respiration can also be overridden by the coordinating centre. This is why we can’t hold our breath to death. When we try to hold our breath for too long, the brain stem inhibits the cerebral cortex’s overriding ability, and we end up passing out instead.
Test Your Knowledge
Real-Life Scenario:
Freedivers dive down to the depths of water systems to see the beauty of the ecosystems undisturbed by scuba-related distractions. In this situation, the divers have to practice voluntary respiration multiple times to be able to hold their breath for enough time to dive down and enjoy the ecosystem with enough remaining air to return to the surface. In this situation describe how practicing voluntary respiration allows these divers the ability to hold their breath for longer periods of time. Why does involuntary respiration not step in to override their efforts? Hint: Think about the brain centres that are involved in these processes.
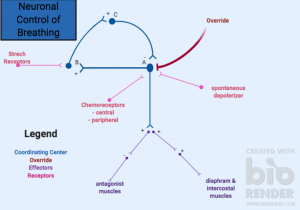
Let’s walk through the pathway in figure 1 together! To start, let’s take a look at what happens at the level of the coordinating centre. A spontaneous depolarizer synapses onto neuron A, causing the neuron to fire. In this diagram, the coordinating centre contains a series of three linked neurons, which feedback onto neuron A to inhibit it, creating a negative feedback loop. Depolarization in neuron A signals to effectors, leading to inspiration. It does this by exciting respiratory muscles, like the diaphragm, to stimulate inhalation and inhibit muscles that antagonize this process. The override system located in the brain stem also synapses onto neuron A. This allows the brain to control respiration consciously and unconsciously through external signal receptors. These signaling complexes detect outside factors and feedback onto the coordinating centre to control breathing.
This exercise below provides a quick review of all the components involved in voluntary respiration. If you have difficulty completing this drag and match activity, it’s recommended that you pause to take some time to walk through the pathway again. This activity is suitable for learners that want to test their knowledge.
Did you know that different parts of the brainstem mediate different aspects of breathing? The respiratory centres of the brain stem are spread throughout the medulla and pons; however, several distinct anatomical regions can be described, and each region contributes to the control of respiration in a functionally unique way. There are many resources to find out more about the brain stem functions to help your learning!
Tip From Past Students
Try drawing out the pathway for neuronal control without your notes and see what you can remember! Don’t just memorize the pathways or cascade events talked about further in this chapter. It is important to make sure you understand each connection as it is crucial for integration.
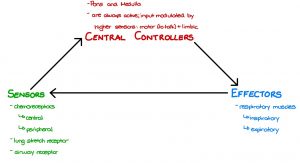
Sensors
A negative feedback response regulates respiration. There are three main components of negative feedback responses: the sensor, the coordinating centre, and the effector. Therefore, in respiration, the coordinating centre is the brain stem. The effectors are the diaphragm and external intercostal muscles. The sensors are the chemoreceptors, stretch receptors, high-pressure baroreceptors, and irritant receptors (Figure 2).
Chemoreceptors
Chemoreceptors are specialized sensory receptors that convert a chemical substance into a biological signal. If the chemoreceptor is a neuron, this signal may be in the form of an action potential. In this example, the action potential travels along the nerve pathways and feedback to different areas of the brain.
Although there are many types of chemoreceptors, only a few are involved in respiration. Respiratory chemoreceptors detect blood carbon dioxide levels by monitoring the concentration of hydrogen ions in the blood. An increase in carbon dioxide results in a decreased blood pH due to hydrogen ion production from carbonic acid. Therefore, these receptors can use pH to measure the level of carbon dioxide in the blood. There are two main chemoreceptors involved in this respiratory feedback look, and they are denoted based on their locations within the body. Central chemoreceptors are found within the brain and detect pH changes in the cerebral spinal fluid. In contrast, peripheral chemoreceptors are located in the carotid artery, specifically denoted as carotid bodies, as well as the aortic arch, where they are referred to as aortic bodies. The carotid bodies can detect changes in oxygen, carbon dioxide, and pH levels. However, the aortic bodies can only detect blood gases, oxygen, and carbon dioxide. They cannot sense changes in pH.
Test Your Knowledge
Clinical Application:
Diabetic individuals can sometimes fall into a state of metabolic acidosis when their blood glucose levels drop dramatically. This leads to a three-fold increase in ketone production and an increase in blood pH. How would this change in blood pH affect the respiratory system? How might their lungs try to compensate for this physiological state? Hint: Compare and contrast central and peripheral chemoreceptors and be sure to understand what they will trigger when they try to return to an average blood pH.
As previously mentioned, in respiration, the chemoreceptors act as sensors in the negative feedback response. To better understand this feedback loop, let’s take a look at a few scenario-based examples.
Consider the case of hypercapnia, which is when you have too much carbon dioxide in your bloodstream. This usually happens as a result of hypoventilation or not being able to breathe correctly. To compensate for this increased level of carbon dioxide, the chemoreceptors will stimulate an increase in PaCO2, which will increase the action potential frequency from sensors in the body to the coordinating centre. This will increase ventilation, including an increase in the frequency and depth of breaths taken.
Now, let’s consider the case in which a person is hyperventilating. Their increased hyperventilation will remove too much carbon dioxide from their body. As a result of this, there will be less carbonic acid in the blood, and so the concentration of hydrogen ions will decrease, and the blood pH will rise. In this scenario, the chemoreceptors will decrease PaCO2 and decrease the action potential frequency of sensors to the coordinating centre. Overall, leading to a decrease in ventilation and, in turn, a decrease in the frequency and depth of breaths taken.
Interestingly, central chemoreceptors can be desensitized over time due to chronic decrease in the amount of oxygen available to tissues, also known as hypoxia. However, peripheral chemoreceptors do not desensitize over time, but their effect on ventilation is less than that of central chemoreceptors.
Test Your Knowledge
Clinical Application:
It’s important to note that chemoreceptors also adjust for oxygen levels to prevent hypoxia. What cascade of events will happen within this situation? Hint: Only the peripheral chemoreceptors can sense changes in oxygen levels in the blood.
Stretch Receptors
Stretch receptors are mechanoreceptors that respond to mechanical stretch or distortion. Respiratory stretch receptors are located in the trachea and bronchioles and are excited when they are physically manipulated.
During inspiration, the lungs are inflated to their maximum volume. The stretch receptors respond to the mechanical distortion and send an action potential signal to the brain stem or coordinating center. This will act to inhibit the inspiratory neurons and decrease the respiratory rate. This is also known as the Hering-Breuer reflex, which is triggered to prevent the over-expansion of the lungs.
During expiration, the lungs begin to deflate, and the stretch receptors are deactivated. The inhibitory signals stop, and inhalation starts again. This is also known as the deflection reflex. Interestingly, these receptors are not active during quiet breathing when the tidal volume is 500 mL. They only become active when the tidal volume is greater than 800 mL, such as during exercise.
This matching activity is for you to have a learning break and test your knowledge of respiratory sensors. If any aspect of this activity is challenging, it is recommended that you take the time to review the different receptors and their functions again.
High-Pressure Baroreceptors
High-pressure baroreceptors are mechanoreceptors that respond to changes in the tension of arterial walls. They are located in the carotid sinus and aortic arch and are sensitive to high blood pressure. When there is a decrease in mean arterial pressure (MAP), a cascade event is triggered. Firstly, there is an increase in action potential frequency from the high-pressure baroreceptors to the coordinating centre. This leads to an increase in ventilation, including an increase in the frequency of breathing and depth of breathing.
Irritant Receptors
Irritant receptors are sensors located on airway epithelium that are sensitive to chemical agents and particles. These receptors respond to both mechanical and chemical stimuli.
Inhalation of toxic chemicals will inhibit ventilation. Inhalation of foreign particles will inhibit ventilation and also stimulate a cough reflex. These receptors are important because they protect the lungs from harmful chemicals and foreign particles.
Key Takeaways
Consider the following concepts to help guide your studies:
- Voluntary respiration is controlled in the cerebral cortex and can override involuntary breathing activities directed in the coordinating centre.
- Stretch receptors in the respiratory tract, chemoreceptors, and spontaneous depolarizers stimulate the brain’s coordinating centre.
- Respiratory chemoreceptors regulate the level of carbon dioxide within the blood by monitoring hydrogen ions present within the blood.
- Stretch receptors are triggered during moments of exercise to increase ventilation.
- High pressure-baroreceptors are triggered by a mechanical stretch of the aorta related to mean arterial pressure changes.
- Irritant receptors are utilized to prevent toxic substances from entering the airway.
Subchapter Quiz
The questions below have been created to assess your knowledge within this subchapter. You will find multiple-choice questions as well as open-ended questions to test your understanding. The multiple-choice questions will provide you with responses to your answers. However, the open-ended questions will be for you to judge, so be sure to check over your answers to see if you are missing any critical points after you’ve completed them.
Media Attributions
- Neuronal Control of Breathing © Sarah Fitzgerald is licensed under a CC BY (Attribution) license
- Respiratory Centres © Leah Martin is licensed under a CC BY-ND (Attribution NoDerivatives) license
Located in the carotid artery and aortic arch.
Located in the brain, detect pH changes in cerebral spinal fluid.
Respiration that occurs without conscious control.
Controls the body's involuntary and metabolic functions.
Sensory receptor cells that are sensitive to changes in the physiological chemical properties (ie. pH).
Respiration that occurs under conscious control.
Occurs when some function of the output of a system, process, or mechanism, is fed back in a manner that tends to reduce the output.
A change in membrane potential that passes along a neuron or muscle fiber to transmit an impulse.
Excessive amounts of CO2 (carbon dioxide) in the bloodstream.
Breathing at an abnormally slow rate.
Rapid and deep breathing.
Not enough oxygen to properly function.
Mechanoreceptors that respond to mechanical stretch or distortion.
A reflex that is triggered to prevent the over-expansion or inflation of the lungs.
Mechanoreceptors that respond to changes in the tension of arterial walls.
Sensors that respond to both mechanical and chemical stimuli and protect the lung from harmful chemicals and foreign particles.

