Secretions
Now that we have learned the general anatomy, directionality, and electrophysiology of the gastrointestinal tract, it is time to focus on the critical chemical processes that make digestion and absorption possible. Various secretions are constantly entering the lumen of the gastrointestinal tract at many different sites. While reading this chapter, it is important to remember the idea of directionality and anatomy of the epithelial tissue.
Learning Outcomes
In this section, you will learn…
- The names of many important secretions.
- The location of where each secretion is produced and their mechanism of secretion.
- The function and target of each secretion.
- The role of accessory organs.
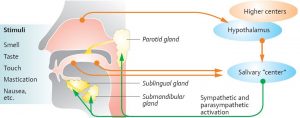
Salivary
The very first secretion that food encounters on its way through the gastrointestinal tract is in the mouth. Digestion begins immediately once food enters the mouth! Think about saliva production as a feedback loop: once food enters the mouth the brain reacts and communicates with the salivary glands to produce saliva. Take a look at figure 1 which illustrates the level of complexity of the interactions between the brain and salivary glands.
Try the following question below to test your knowledge!
Gastric
Once food travels down the esophagus into the stomach, it initiates many more secretions. Though the stomach is typically thought of as a storage container, it actually does much more! From its stunningly low pH to its power to muscularly contract, the stomach serves an important role in the chemical and mechanical digestion process of food. In this section, we will focus on the secretions from the stomach – known as gastric secretions.
Cell Types
The lining of the stomach is perforated with gastric pits. Gastric pits are invaginations in the surface epithelium that contain gastric glands. These glands are responsible for the production and secretion of the various components of gastric juice. The cell types found in the gastric glands are parietal cells, chief cells, G cells, D cells and Enterochromaffin-like (ECL) cells. Take a look at figure 2 below which illustrates the anatomy of the stomach including the various cell types and where they are located.
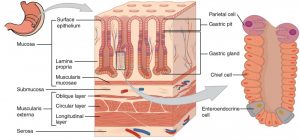
Try not to focus on memorizing the anatomy of the stomach, but think about its functional organization. Why are certain cell types located where they are? How is their location related to their function?
Test Your Knowledge
Thinking Beyond:
You’re preparing for a major test and your friend is rapid-firing the following questions at you: Which cell types are found in the gastric pits? Name one cell type that is found closer to the top of the gastric pit and why is it found there? Explain the role of chief cells and G cells in detail, compare and contrast them. Hint: Think about the functional organization of the stomach wall while answering the following.
Gastric Juices
Gastric juice is made up of digestive enzymes, hydrochloric acid and other substances that are important for absorbing nutrients. The hydrochloric acid in the gastric juice breaks down the food and the digestive enzymes split up the proteins into smaller polypeptide segments. Take a look at Table 1 which outlines the components of gastric juice, where they are produced, what stimulates their production and their functions. [1]
| Gastric juice component | Production site | Production stimulus | Target organ or molecule | Action |
|---|---|---|---|---|
| Hydrochloric acid (HCl) | Parietal cells | Hormonal and neural inputs | Proteins, micro-organisms, pepsinogen | Kills micro-organisms, denatures proteins, activates pepsinogen |
| Pepsinogen | Chief cells | Hormonal and neural inputs | Proteins | Digests polypeptides in peptide segments |
| Gastrin | G-cells | Presence of peptides and amino acids in stomach | Chief and parietal cells | Increases secretion from gastric glands, promotes gastric emptying |
| Somatostatin | D-cells | Presence of food in stomach; sympathetic axon stimulation | Stomach, small intestine, pancreas | Inhibits all gastric secretions, gastric mobility and gastric emptying |
| Histamine | ECL-cells | Presence of food in the stomach | Parietal cells | Stimulates parietal cells to secrete HCl and intrinsic factor |
Mucosal Lining
As you probably know, the stomach is a highly acidic environment. Therefore, the cells of the stomach require protection from destruction and damage. The stomach is protected from self-digestion by the mucosal barrier. This barrier has several components. First, the stomach wall is covered by a thick coating of bicarbonate-rich mucus. This mucus forms a physical barrier, and its bicarbonate ions neutralize acid. Stem cells quickly also produce new stomach cells. In fact, the surface epithelium of the stomach is completely replaced every 3 to 6 days. [3]
Parietal Cell
Hydrochloric acid (HCl) denatures incoming proteins from foodstuffs and kills harmful bacteria that may enter the gastrointestinal tract. It is produced by parietal cells. Take a look below at the diagram, textual description and video that examine the mechanism of hydrochloric acid secretion from parietal cells.
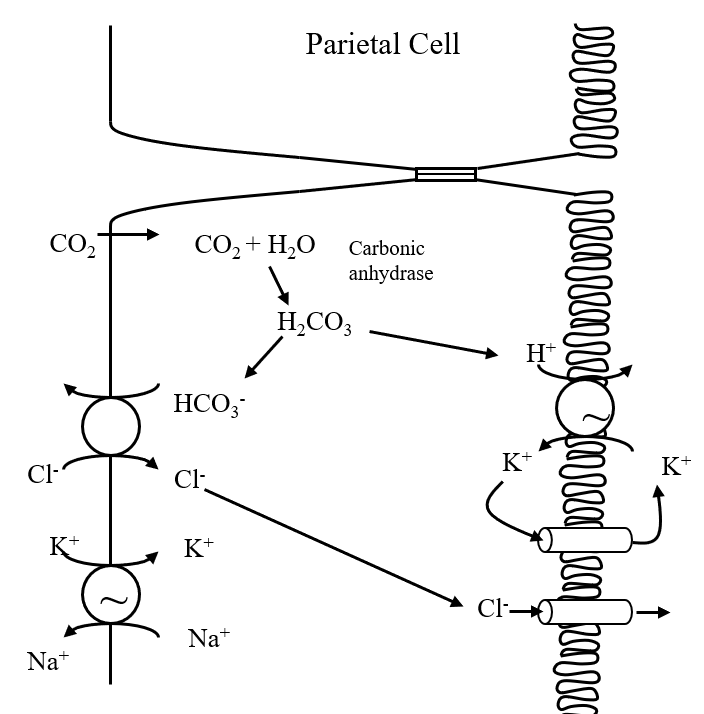
Hydrochloric acid secretion by the parietal cell involves separation of H+ (hydrogen) ions which are released into the gastric lumen and HCO3− (Bicarbonate) released into the blood. CO2 (carbon dioxide) diffuses into the cell from plasma or is produced by cellular metabolism. It becomes hydrated to H2CO3 (carbonic acid), a process facilitated by the enzyme carbonic anhydrase. H2CO3 dissociates into H+ and HCO3−. At the apical membrane H+ is transported out of the cell in exchange for K+ (potassium) by the H+/K+ ATPase also known as the “Proton pump.” The K+ taken into the cell recycles back out into the gastric lumen via a K+ channel, resulting in the elevated K+ concentration of gastric juice. The final component of gastric HCl is Cl– (Chloride) which exits passively through a Cl– channel. Thus, the apical H+-K+ ATPase drives the secretion of HCl. [4]
The video below shows how parietal cells produce hydrochloric acid from 0:03-3:29.
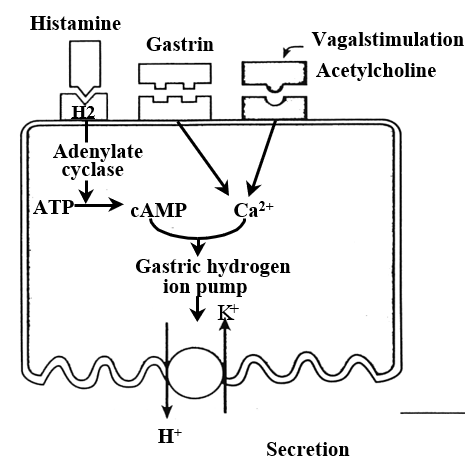
The production and secretion of hydrochloric acid is controlled by several factors, which act via paracrine, endocrine, or neuronal action, as shown in figure 5, but don’t worry about the bottom right corner image about potentiation. Ask yourself, where do all these inputs come from?
We also must consider the impact of inhibitory inputs. Somatostatin acts on a specific receptor which is coupled to an inhibitory G protein and inhibits adenylate cyclase and thereby the effect of histamine [5]
Test Your Knowledge
Thinking Beyond:
Parietal cells secrete hydrochloric acid. Explain how the following events would increase or decrease hydrochloric acid secretion. Increased activity of the PNS? Increased activity of ECL cells? Increased activity of D cells? Hint: Think about what stimulus comes from each event and what the body would do in these situations.
Consider the video below which illustrates where all the substances are coming from, as well as their mode of action (i.e. endocrine, paracrine, etc.) as seen from 4:13-7:35. The section where arachidonic acid is discussed is purely to show where prostaglandins in your notes come from. You do not need to know anything about arachidonic acid as it beyond the scope of the course. It is also important to note that the K+ and Cl− transporters on the apical membrane are shown differently in this video; they are shown as one transporter, whereas in the notes, they are separate.
Take some time to try the following question below to test your knowledge!
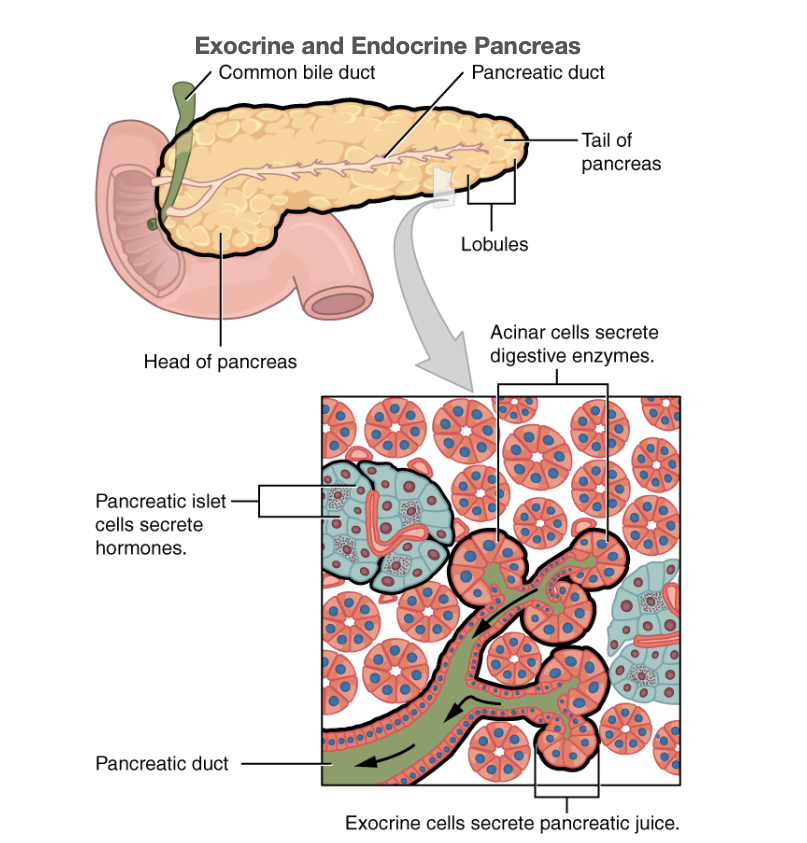
Pancreas
The pancreas is a vital organ and is responsible for secretion and production of insulin and glucagon, two very important hormones when it comes to energy status. In type 2 diabetes, the body is either insulin resistant (doesn’t respond to insulin properly) or the pancreas is no longer able to produce enough insulin. This leads to poor glucose management, which is a vital fuel for the body.
Every wonder why diabetics cannot control blood glucose levels? In type 2 diabetes, the body is either insulin resistant (doesn’t respond to insulin properly) or the pancreas is no longer able to produce enough insulin. This leads to poor glucose management, which is a vital fuel for the body.
Secretions
There are two types of pancreatic secretions which include the aqueous component containing HCO3− which comes from pancreatic duct cells and the enzymatic component which comes from acinar cells. Regulation of pancreatic secretion is the job of hormones. The entry of acidic chyme into the duodenum stimulates the release of the hormone secretin, which in turn causes the duct cells to release bicarbonate-rich pancreatic juice. The presence of proteins and fats in the duodenum stimulates the secretion of the hormone CCK, which then stimulates the acini to secrete enzyme-rich pancreatic juice and enhances the activity of secretin. [6]
Aqueous component
Remember that food has now traveled from the stomach to the small intestine. The stomach is highly acidic, and therefore the food product entering the small intestine is as well (pH=2). The role of the aqueous component is to bring HCO3− (bicarbonate) into the small intestine. To understand the role of this component, consider what would happen when HCO3− mixes with the acidic food. Due to the fact that HCO3− is a basic compound, it will work to neutralize the acidic food components The key point to remember is that the aqueous component is not digestion focused, the enzymatic component is what contains enzymes that help to break down proteins.
Enzymatic Component
The pancreas produces protein-digesting enzymes in their inactive forms. These enzymes are activated in the duodenum. If they were produced in an active form, they would digest the pancreas (which is exactly what occurs in the disease, pancreatitis).The enzymes that digest starch (amylase), fat (lipase), and nucleic acids (nuclease) are secreted in their active forms, since they do not attack the pancreas as do the protein-digesting enzymes. [7]
Try the following question below to test your knowledge!
Liver
The liver, another accessory organ, has vital secretions when it comes to the digestion of lipids. The focus of this section is on bile, specifically its secretion, role, and circulation. This, like the pancreas, makes its secretions through the Sphincter of Oddi into the duodenum.
The blood that reaches the liver contains substances that it has picked up while traveling towards the liver. The liver hepatocytes are able to remove substances in blood as it passes through the liver. These substances can be sent from the hepatocytes into the bile canaliculus towards to bile duct for excretion. The portion that is excreted into the small intestine is known as bile.
Bile
Recall that lipids do not dissolve in water. Thus, before they can be digested in the watery environment of the small intestine, large lipid globules must be broken down into smaller lipid globules, a process called emulsification. Bile is a mixture secreted by the liver to accomplish the emulsification of lipids in the small intestine.
Hepatocytes secrete a yellow-brown or yellow-green solution of water, bile salts, bile pigments, cholesterol, and other molecules known as bile. The bile salts are the most critical for emulsification, which results in the large lipid globules being pulled apart into many tiny lipid fragments This change dramatically increases the surface area available for lipid-digesting enzyme activity. This is the same way dish soap works on fats mixed with water! Take a look at figure 7 below which illustrates a simplistic version of emulsification. As you can see, the bile acids (in green) cause the breakdown of the larger lipid globule to increase the surface area for enzymes to attach.

Secretion of Bile
There are two fundamentally important functions of bile in all species. Firstly, bile contains bile acids, which are critical for the digestion and absorption of fats as well as fat-soluble vitamins in the small intestine. Secondly, many waste products are eliminated from the body by secretion into bile for elimination in feces. Adult humans produce 400 to 800 mL (milliliters) of bile daily, and other animals produce proportionately similar amounts. The secretion of bile can be considered to occur in two stages. Initially, hepatocytes secrete bile which flows into bile ducts. This hepatic bile contains large quantities of bile acids, cholesterol and other organic molecules. Then, as bile flows through the bile ducts it is modified by the addition of a watery, bicarbonate-rich secretion from ductal epithelial cells. The gall bladder then stores and concentrates bile during the fasting state. Typically, bile is five times as concentrated in the gall bladder by absorption of water and small electrolytes. Virtually all of the organic molecules are retained.
Role of Bile Acids in Fat Digestion and Absorption
Bile acids are derivatives of cholesterol from the diet as well ashepatic synthesis which are synthesized in the hepatocyte. Bile acids are amphipathic, that is, they contain both non-polar (hydrophobic) and polar (hydrophilic) segments. The cholesterol-derived portion of a bile acid has one face that is hydrophobic (methyl groups) and one that is hydrophilic (hydroxyl groups). The structure of bile acid is shown in figure 8 below.
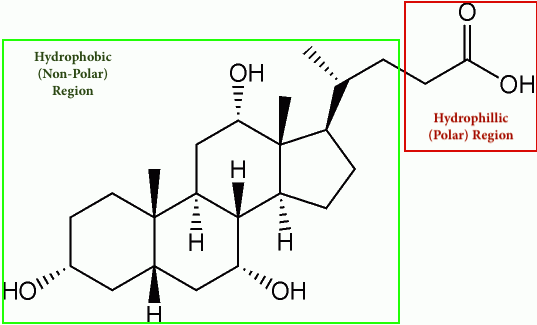
Their amphipathic nature enables bile acids to carry out two important functions. The first of which is the emulsification of lipid aggregates. Bile acids have detergent action on particles of dietary fat which causes fat globules to break down or be emulsified into minute, microscopic droplets. Emulsification is not digestion per se but is of importance because it greatly increases the surface area of fat, making it available for digestion by lipases, which cannot access the inside of lipid droplets. The second function is the solubilization and transport of lipids in an aqueous environment. Bile acids are lipid carriers and are able to solubilize many lipids by forming micelles – aggregates of lipids such as fatty acids, cholesterol and monoglycerides – that remain suspended in water. Bile acids are also critical for the transport and absorption of fat-soluble vitamins.
Role of Bile Acids in Cholesterol Homeostasis
Hepatic synthesis of bile acids accounts for the majority of cholesterol breakdown in the body. In humans, roughly 500 mg of cholesterol are converted to bile acids and eliminated in bile every day. This route for elimination of excess cholesterol is probably important in all animals, but particularly in situations of massive cholesterol ingestion [8]
Bile acid breaks down cholesterol, so bile acid sequestrants, or separators, just help these acids along. The sequestrants take cholesterol-containing bile acids and form them into an insoluble complex — meaning it can’t be dissolved in the body — which then leaves your body through your stool.
Enterohepatic Recirculation
Large amounts of bile acids are secreted into the intestine every day, but only relatively small quantities are lost from the body. This is because approximately 95% of the bile acids delivered to the duodenum are absorbed back into the blood within the ileum. Figure 9 illustrates the path of bile acids in the recycling process.
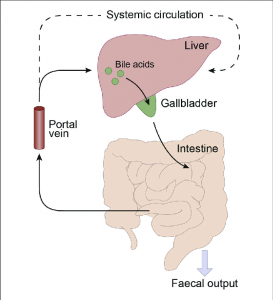
Venous blood from the ileum goes straight into the portal vein, and hence through the sinusoids of the liver. Hepatocytes extract bile acids very efficiently from sinusoidal blood, and little escapes the healthy liver into systemic circulation. Bile acids are then transported across the hepatocytes to be re-secreted. The net effect of this enterohepatic recirculation is that each bile salt molecule is reused about 20 times, often two or three times during a single digestive phase.
Try the following question below to test your knowledge!
Control of Bile Secretion
The flow of bile is lowest during fasting, and a majority of that is diverted into the gallbladder for concentration
When chyme from an ingested meal enters the small intestine, acid and partially digested fats and proteins stimulate the secretion of cholecystokinin and secretin. The name of cholecystokinin describes its effect on the biliary system as cholecysto = gallbladder and kinin = movement. The most potent stimulus for the release of cholecystokinin is the presence of fat in the duodenum. Once released, it stimulates contractions of the gallbladder and common bile duct, resulting in the delivery of bile into the gut. Secretin is secreted in response to acid in the duodenum. Its effect on the biliary system is very similar to what was seen in the pancreas as it simulates biliary duct cells to secrete bicarbonate and water, which expands the volume of bile and increases its flow out into the intestines.
Small Intestine
Just like the mouth, stomach, and accessory organs, the small intestine makes a variety of contributions to the substances that allow digestion to occur. The small intestine is the largest endocrine organ and plays a critical role in gastrointestinal tract secretions.
Cell Types
The small intestine has multiple types of cells that all make different secretions. Some of these cells are similar or the same as cells you have previously learned about in other organs, but some are unique to the small intestine.
| Secretion | Production Site | Production Stimulus | Action |
|---|---|---|---|
| Mucous | Goblet cells | Sight/Smell/Thought of food | Moisten food, begin digestion |
| Cholecystokinin (CCK) | I cells | Presence of food | Promotes insulin/glucagon secretion (feed forward mechanism) |
| Secretin | S cells | Presence of food | Promotes insulin/glucagon secretion (feed forward mechanism) |
| Somatostatin | D cells | Presence of food | Inhibits gastric secretions, gastric mobility, and gastric emptying |
| Glucose-dependent insolinotropic peptide (GIP) | K cells | presence of glucose in the duodenum | stimulates insulin release |
| Motilin | Endocrine cells | Presence of food | changes the membrane potential (frequency and pattern of action potentials) and increases motility |
| Glucagon-like peptide 1 (GLP-1) | Endocrine cells | Glucose in the duodenum | simulates insulin release |
| Bulbogastrone | Endocrine cells | presence of acid in the duodenum (pH too low) | Decreases HCl secretion of parietal cells in the stomach to raise pH (endocrine function) |
| Entero-oxyntin | Endocrine cells | stimulates gastric acid secretion (in the stomach) | |
| Enteropeptidase (enterokinase) | Secretory cells | Convert trypsinogen into trypsin |
Tips From Past Students
Throughout the chapter, you often see tables with a list of secretions, cell types, and actions. Focus on secretions that are either common between organs, or work to inhibit or stimulate other secretions. Look for common themes throughout to help you remember.
I cells and S cells
I cells and S cells have different secretions, but share similar functions. Both are part of a feed-forward mechanism. The secretions are stimulated by the presence of food that has been partially digested and is mixed with chyme in the small intestine. In turn, these secretions signal the release of pancreatic enzymes and bile. They can also act on the alpha and beta receptors of the pancreas, which secrete insulin (in a fed state) and glucagon (in a fasted state).
Endocrine cells
Endocrine cells have multiple secretions including motilin, Glucagon-like peptide 1 (GLP-1) and bulbogastrone. Motilin has the ability to change the membrane potential of cells. This change increases the spike potential frequency and pattern, which will generate more force. This increases motility in the small intestine by increasing the force and frequency of segmental contractions. If this doesn’t make sense to you, then it would be helpful to go back and read the Electrophysiology and Gastrointestinal Motility sections of the Structure and Mobility subchapter. Glucagon-like peptide 1 acts on the pancreas to increase insulin release. It is stimulated by the presence of glucose in the small intestine and helps increase the uptake of glucose into epithelial cells. GLP-1 is what we call an incretin. It is made further down in the small intestine (jejunum, ileum) and also in the colon. GLP-1 and other incretins act on the beta cells of the pancreas to depolarize them and increase the secretion of insulin when signaled by glucose. Increasing the amount of insulin secreted causes the body’s blood glucose levels to lower back down to a normal level after a meal. Incretins are key regulators of the body’s blood glucose homeostasis. This is beyond the level of this course, but many of you will learn about the role of GLP-1 and other incretins in other classes. Lastly, bulbogastrone is secreted by endocrine cells in the small intestine but will act on the stomach. When acid begins to accumulate in the small intestine, causing the pH to drop, it will signal to the parietal cells of the stomach to slow their production of HCl. This will ensure that the pH of the small intestine doesn’t get too low, as an environment that is too acidic can be quite harmful.
Secretory Cells
The small intestine works closely with secretions from the pancreas since the pancreatic duct empties into the duodenum. As you learned in the pancreatic secretions section above, the pancreas secretes zymogens (inactive enzymes) such as trypsinogen, chymotrypsinogen, proelastase, and procarboxypeptidase. The small intestine has secretory cells which release enteropeptidase (also called enterokinase), which sits on the brush border. Enteropeptidase will convert trypsinogen into trypsin, and then trypsin will convert the other zymogens into proteases.
Key Takeaways
Real-Life Scenario:
You have a rare disease where your small intestine does not secrete enteropeptidase. How and why would this affect the levels of zymogens, proteases and peptidases in the small intestine? Hint: Think back to the secretions learned about in this unit and how they can affect the body.
Try the following question below to test your knowledge!
The brush border also has a group of peptidases (aminopeptidase, dipeptidase, and dipeptidyl aminopeptidase). They are not secreted by the secretory cells of the small intestine, but it is important to note they are present here to finish off the job that proteases started. The difference between proteases and peptidases is that proteases break down larger proteins first, then peptidases break down the small peptides into single amino acids or oligopeptides. You will learn more about this in the next section, Digestion and Absorption.
Key Takeaways
Consider the following concepts to help guide your studies:
- Understanding the function and target of each secretion.
- How the stomach is involved in the chemical and mechanical digestion process of food.
- How the Liver is vital is involved in the digestion of lipids.
Subchapter Quiz
The questions below can be used to assess your knowledge within this chapter. There are multiple-choice questions that you should attempt without referring to your notes. The questions will provide you with responses to your answers to guide your studying but should not be used as your only resource.
Media Attributions
- Salivary Secretion Communication © Roger TannerThies is licensed under a All Rights Reserved license
- Stomach Histology © Donna Browne is licensed under a CC BY (Attribution) license
- Mucosal © Thomas Schwenke is licensed under a All Rights Reserved license
- Mechanism of HCl Secretion by Parietal Cells © John Williams, M.D., Ph.D. is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- Receptors and Intracellular Messengers Regulating Parietal Cell H+ Secretion © John Williams, M.D., Ph.D. is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- The Pancreas © Rice University is licensed under a CC BY (Attribution) license
- Emulsification of lipids © Joshua Thomas is licensed under a CC BY-NC (Attribution NonCommercial) license
- Cholic Acid © Shaddack is licensed under a All Rights Reserved license
- Enterohepatic Circulation © Kim Mertens, Andries Kalsbeek, Maarten Rene Soeters and Hannah M. Eggnik is licensed under a CC BY (Attribution) license
- How does the stomach work? (2016, August 21). Retrieved April 12, 2021, from https://www.ncbi.nlm.nih.gov/books/NBK279304/ ↵
- Digestive System Module 4: The Stomach. (n.d.). Retrieved April 12, 2021, from https://cnx.org/contents/3xzxwV_7@1.1:24bUfgSh@2/Digestive-System-Module-4-The-Stomach . ↵
- Digestive System Module 4: The Stomach. (n.d.). Retrieved April 12, 2021, from https://cnx.org/contents/3xzxwV_7@1.1:24bUfgSh@2/Digestive-System-Module-4-The-Stomach ↵
- Williams, J. (2009). GI Sequence - Stomach. Retrieved April 11, 2021, from https://open.umich.edu/sites/default/files/downloads/j.williams.giphys.4-stomach-38-65-notes.pdf ↵
- Williams, J. (2009). GI Sequence - Stomach. Retrieved April 11, 2021, from https://open.umich.edu/sites/default/files/downloads/j.williams.giphys.4-stomach-38-65-notes.pdf ↵
- Digestive System Module 6: Accessory Organs in Digestion: The Liver, Pancreas, and Gallbladder. (n.d.). Retrieved April 12, 2021, from https://cnx.org/contents/3xzxwV_7@1.1:l68JiflN@1/Digestive-System-Module-6-Accessory-Organs-in-Digestion-The-Liver-Pancreas-and-Gallbladder ↵
- Digestive System Module 6: Accessory Organs in Digestion: The Liver, Pancreas, and Gallbladder. (n.d.). Retrieved April 12, 2021, from https://cnx.org/contents/3xzxwV_7@1.1:l68JiflN@1/Digestive-System-Module-6-Accessory-Organs-in-Digestion-The-Liver-Pancreas-and-Gallbladder ↵
- VIVO Pathophysiology. (n.d.). Retrieved April 12, 2021, from http://www.vivo.colostate.edu/hbooks/pathphys/digestion/liver/eateggs.html ↵
The formation of a circuit in which outputs of a system route back as inputs promoting cause-and-effect. The system can either be amplified (positive) or inhibited (negative feedback).
Distant cell signals that utilize the circulatory system to emit a slow and long-lasting response.
An anabolic hormone that allows glucose uptake into cells.
A catabolic hormone which promotes the increase of glucose in the bloodstream by converting glycogen stores in liver to glucose via glycogenolysis.
The body is unable to utilize synthesized insulin properly or it can’t make enough insulin. As a result, blood sugar levels increase.
Pancreatic cells that synthesize and transport enzymes to aid in food digestion in the duodenum.
Process that aids in lipid digestion. Lipids are prevented from aggregating/clumping causing the hydrophobic molecules (lipids) to be evenly dispersed in a hydrophilic environment. This is because bile salts, which are amphipathic, surround the small lipid molecules.
Cells in the liver that play a role in metabolism, protein synthesis, and detoxification.
Minerals in the blood, tissues, urine, and other bodily fluids that contain an electric charge. Electrolytes balance the body’s pH levels as well as the amount of water in the body.
Contains both hydrophilic (water-loving) and hydrophobic (water-fearing) components.
The process in which a substance becomes soluble or more soluble than it was.
Aggregates of lipids such as fatty acids and monoglycerides.
Low pressure blood vessels that deliver portal and arterial blood to central veins.
The circuit that provides oxygenated blood to the entire body, except the lungs (blood moving to and from the lungs is considered pulmonary circulation).