Anatomy of the Respiratory Tract
Understanding the structure of the respiratory tract is essential for understanding all the significant alterations that contribute to its function. In this chapter, we will dive into the respiration system's anatomy to understand each component's overall structure and function. Some real-life examples help stimulate content application, allowing you to see how diseases or dysfunctions in the anatomy can lead to drastic physiological changes.
Learning Outcomes
In this section you will learn...
- The main structures of the respiratory system.
- The anatomical organization of all respiratory structures.
- The functions of all anatomical structures.
- The basics of breathing in relation to pleural pressure, alveolar pressure, and atmospheric pressure.
Anatomy of Respiration
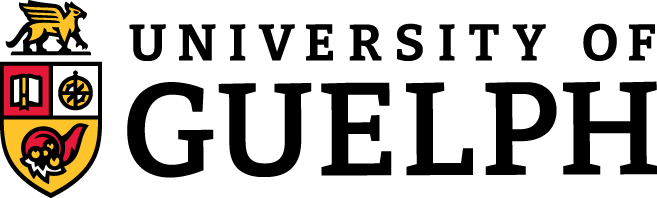
Before we dive into the physiology of respiration, we need to understand the respiratory system's anatomy. After all, the structure of an organism is related to its function. The respiratory system begins at the nose and mouth, continues to the trachea, into the lungs, and the diaphragm, shown in figure 1. The respiratory system's anatomy can be divided into categories based on location within the body: the upper and lower respiratory tracts. The upper respiratory tract includes the portion of the larynx above the vocal folds, and the lower respiratory tract consists of the portion of the larynx below the vocal folds.
Let's take some time and review the major structures within the upper and lower respiratory tracts with this activity!
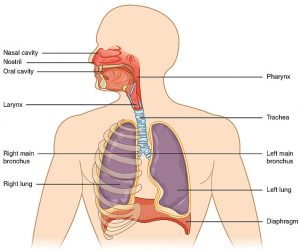
The second way to categorize the respiratory system is by dividing structures into two areas: the conducting region and the respiratory zone. The conducting area includes the nose, mouth, pharynx, paranasal sinuses, larynx, trachea, primary, secondary, and tertiary bronchi and bronchioles. These structures form a continuous route to allow the passage of air into and out of the lungs. This zone is mainly responsible for removing foreign particles and pathogens from incoming air as well as warming and moistening the air before it goes into the lungs. The passage of air, shown in figure 2, can be described as it begins in the mouth or nose and travels down the trachea, through the various bronchi, and into the alveoli. The trachea splits into two main bronchi, the right and left primary bronchi. The two primary bronchi are then further divided into secondary bronchi, then tertiary bronchi. After the first three generations of bronchi, the airways get more narrow, and they are now called bronchioles. The bronchioles branch off into terminal bronchioles, then respiratory bronchioles. Eventually, the respiratory bronchioles end where the alveoli start.
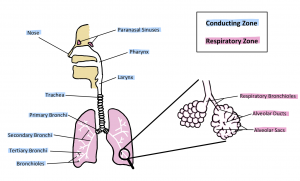
The respiratory zone consists of structures including respiratory bronchioles, alveolar ducts, and alveoli, which are directly involved in gas exchange. The respiratory zone begins when the terminal bronchiole joins with a respiratory bronchiole, as shown in figure 3. The respiratory bronchioles split into several alveolar ducts, which terminate in alveolar sacs that contain a collection of alveoli.
Test Your Knowledge
Thinking Beyond:
The layout of structures in your lung is often referred to as being similar to a tree. Why do you think this would be? What structures would correlate to the tree? Hint: Think about how a tree grows; it starts with a strong trunk before building branches and leaves.
Structures and Characteristics
Understanding the respiratory system’s structural characteristics allows for a deeper understanding of how each part works to help the system function as a whole. This section will focus on the types of cells, tissues, and muscles associated with each structure and will be touched upon again in later sections. Keep these structures and characteristics in mind throughout the unit as they provide clues to how each portion of the respiration pathway responds to the induction and excretion of external atmospheric gases.
To start, let's look at the trachea and bronchi. If you feel the front of your throat, you might notice intermittent bumps. These are cartilaginous rings that provide structure to this tube to prevent collapse resulting from pressure. In between these cartilaginous rings, there are connecting smooth muscle, epithelial and goblet cells. The smooth muscle present helps control the tubes' diameter, while the goblet cells secrete mucous to help facilitate the transport of air down the respiratory tract. Now we transition into the bronchioles, there is a noticeable decrease in the abundance of smooth muscle cells, goblet cells and no cartilage. This is in preparation for the alveoli. The alveoli complete the airflow pathway and end in a single layer of elongated epithelial cells that line the basement membrane separating the blood from the air. This barrier is the site where blood is brought in close proximity to atmospheric air, allowing for efficient gas exchange.
This learning object is included to help students better grasp the anatomy of the respiratory system. The most crucial information within this video can be found between 2:45 - 7:32. This section explains essential characteristics of the trachea, bronchi, bronchioles, and alveoli in great detail. The most important points to remember from the video are the type of cells, tissue, and muscle associated with each structure and how their function influences respiration.
Ever wonder why our lungs are not the same size? Our right lung is broader and shorter than the left lung. The right lung is smaller because it has to make room for the liver, located right underneath it. Similarly, the left lung is narrower than the right lung to accommodate the heart's placement.
Speaking of size, did you know that the right primary bronchus is wider and more vertical than the left primary bronchus? This is essential for foreign particle expulsion. For instance, if you accidentally inhaled something big, it will most likely make its way to the right primary bronchus so that enough air will be present to push the object out through coughing.
Test Your Knowledge
Real-Life Scenario:
It's winter break from school, so you and your friend decide to go on a beautiful snowy hike through the forest. You are walking along a commonly used trail atop a very steep hill. Unknown to you, there is a thick layer of ice hidden under the fresh snow powder. Your friend slips and tumbles down the steep slope. When you reach them, you see a tree branch lodged in their intercostal space. Why is your friend having trouble breathing? How will this create a pressure difference? Hint: The stick has punctured their pleural cavity but not their lung. Read a little further into the next section and come back to this.
Chest Wall and Pleural Anatomy
The primary role of the respiratory system is gas exchange. Breathing, also known as ventilation, is the process of moving air into and out of the lungs to facilitate systemic gas exchange. Having a basic knowledge of chest wall and pleural anatomy is the first step to understanding breathing mechanisms.
The muscles of respiration contribute to inhalation and exhalation by expanding or decreasing the thoracic cavity space. The two main muscles of respiration are the diaphragm and the intercostal muscles. During inspiration, the diaphragm contracts and moves down while external intercostal muscles contract, pulling the ribcage upwards and outwards. This results in an increase in volume in the thoracic cavity. Expiration is the reverse process, as the diaphragm relaxes and moves back to its original position, the external intercostal muscles relax as well. This results in a decrease in the thoracic cavity volume, pushing air out of the system.
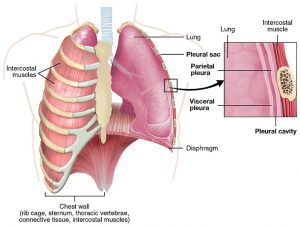
In addition to the muscles of respiration, the pleural cavity also plays an essential role during breathing. The pleural cavity is the thin fluid-filled space between the visceral and parietal pleurae of each lung. The visceral pleura envelopes the lungs, while the parietal pleura attaches to the inner chest wall, as shown in figure 6. Inspiration and expiration are mediated in part by pleural pressure, which is the pressure within the pleural cavity. This mechanism and structures will be discussed in later sections.
Tips From Past Students
The amount of information on respiratory anatomy may seem quite overwhelming. Just remember not to get too caught up in memorizing every little detail about the anatomy. The most important thing is to get a good grasp of the main structures (i.e., trachea, bronchi, bronchioles, alveoli, pleural cavity, and diaphragm), and their characteristics, so that it'll be easier to understand the physiology later on!
Respiratory Flow
Respiratory flow is determined by the magnitude of alveolar pressure and airway resistance. The relationship between airflow, pressure, and resistance is described by the respiratory flow equation where Q is airflow, P1 is the atmospheric pressure, P2 is equivalent to the alveolar pressure and R is the airway resistance. This is a very important equation to know moving forward.
[latex]Q=\frac{P_1 − P_2}{R}[/latex]
Test Your Knowledge
Real-Life Scenario:
Diseases within respiratory tracts can also increase airway resistance. In an asthma attack, airways constrict due to mucosal inflammation and increased contraction of smooth muscles. What would this result in? Why? Hint: Think about how radius and resistance affect breathing.
Atmospheric pressure remains constant at 760 mmHg. For simplicity during calculations, it is often set to 0, and other lung pressures are expressed relative to atmospheric pressure. Alveolar pressure is the pressure in the alveoli which must be negative to get flow during inspiration. If these variables are not sitting well with you now, atmospheric pressure and alveolar pressure will be discussed in greater detail later. Airway resistance is the respiratory tract's resistance to airflow during inspiration and expiration. Although there are a few factors that influence it, the primary control of airway resistance is the radius of the airways, as seen in the equation below. The only variable we need to discuss here is the radius, r, as other variables do not change and you'll notice it is to the fourth power on the denominator. This means that small changes in radius may produce large changes in resistance and, ultimately, respiratory flow. This brings us full circle on this section as we discussed, respiratory flow is partially determined by airway resistance.
[latex]R=\frac{8nl}{\pi r^4}[/latex]
Key Takeaways
Consider the following concepts to help guide your studies:
- The respiratory system can be broken up into two distinct pathways the upper and lower respiratory tracts.
- The tract can be further divided into the conducting zone and the respiratory zone.
- The main cell types that make up the respiratory tract are cartilage, epithelial, smooth muscle, and goblet cells, however, the locations of these cell types vary across the path or airflow.
- The thin basement layer within the alveoli allows for blood to come within close proximity to atmospheric air, allowing for gas exchange to take place.
- The pleural cavity creates a pleural pressure that is essential for breathing.
- Airway resistance and alveolar pressure determine pulmonary flow.
Subchapter Quiz
The questions below can be used assess your knowledge within this chapter. There are five multiple-choice questions that you should attempt without referring to your notes. The questions will provide you with responses to your answers to guide your studying but should not be used as your only resource.
Media Attributions
- Major Respiratory Organs is licensed under a CC BY (Attribution) license
- Conducting and Respiratory Zones © Santana Ferreira is licensed under a CC BY (Attribution) license
- The Lung Pleura is licensed under a CC BY (Attribution) license
The delivery of oxygen from the inhaled air in the lungs into the blood and the removal of carbon dioxide from the blood into the exhaled air in the lungs.
The process of moving air into and out of the lungs to facilitate gas exchange.
Thin fluid-filled space between the visceral and parietal pleurae of each lung.
The air pressure within the pleural cavity that varies during ventilation.
The air pressure inside the lung alveoli that varies during ventilation.
The respiratory tract's resistance to airflow during inspiration and expiration.
The air pressure in the atmosphere at sea level is 760 mmHg. Lung pressures are often expressed relative to this pressure.